Session Information
Date: Tuesday, September 24, 2019
Session Title: Drug-Induced Movement Disorders
Session Time: 1:45pm-3:15pm
Location: Agora 2 West, Level 2
Objective: Present and discuss a case report showing neurotoxicity peripheral and central nervous system–associated with metronidazole use.
Background: Due to the extensive clinical use of metronidazole and the limited recognition of its complications. It is essential to report this case.
Method: Case Report
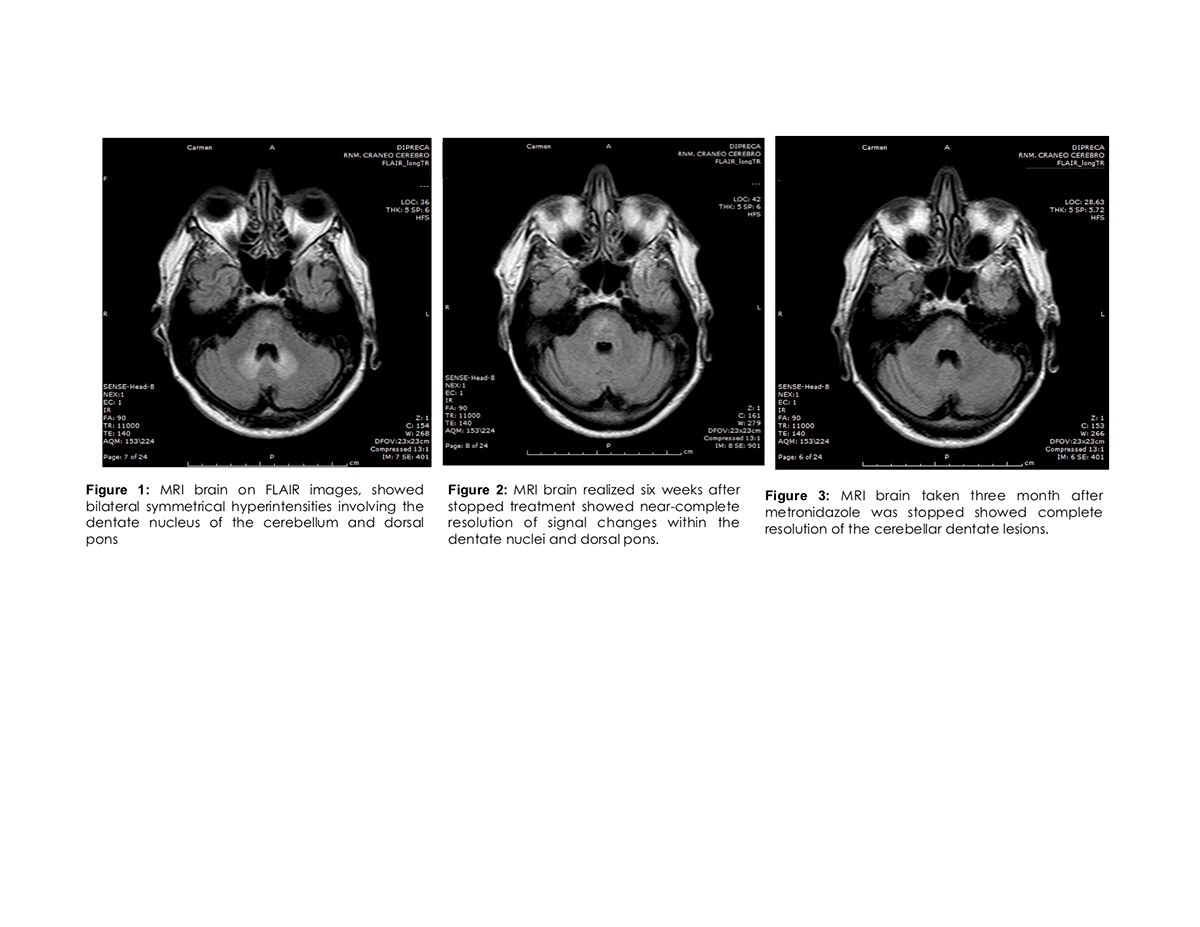
Results: A 79-years-old female presented with a 3 months history of vertigo, slurring of speech and unsteady gait. There was no history of diabetes mellitus or alcohol consumption. She had been taking oral metronidazole 500 mg 3 times a day and ciprofloxacin 500 mg twice a day for a fistulized right psoas abscess and infectious aortitis since 1 month before symptoms. She presented confusion, progressive painful paresthesias involving lower limbs and severe impairment gait of 3 weeks’ duration. On admission, the estimated cumulative metronidazole dose was about 180 g. She was unable to stand or walk. She was disoriented. She had staccato speech. Deep tendon reflexes: ankle were absent with plantar flexor response. She had loss of pinprick sensation below the knees. She presented dysmetria and dysdiadochokinesia and severe trunk and gait ataxia. MRI brain on T2 and FLAIR images showed bilateral symmetrical hyperintensities involving the dentate nucleus of the cerebellum and dorsal pons.(Fig 1) Based on these findings, metronidazole toxicity was suspected, and the drug was discontinued. She experienced a marked improvement evident during the first week. Her orientation, speech and gait returned to normal but a limb burning sensation was not completely relieved. A MRI brain realized 6 weeks after showed near-complete resolution of lesions within the dentate nuclei and dorsal pons.(Fig 2). A MRI brain taken 3 month after showed complete resolution of the cerebellar dentate lesions (Fig 3). Peripheral neuropathy persisted, even 6 months after discharge. In our case, the diagnosis was made clinically, ruling out other clinical and radiological differentials diagnosis and was supported by the MRI findings.
Conclusion: Recognition of metronidazole-induced neurotoxicity depends upon high clinical suspicion, it must be considered whenever a patient using metronidazole experiences a subacute cerebellar syndrome, encephalopathy or polyneuropathy and specific MRI abnormalities of bilateral increased T2/FLAIR signal of the dentate nuclei. The most remarkable feature is complete or near-complete resolution of symptoms and of the original lesions on follow-up MRIs.
References: 1. Yazdani Rana M., Kayfan BS, Samar. MRI findings of metronidazole neurotoxicity in a pediatric patient with chronic diarrhea. Radiology Case Reports 14 (2019) 75–78 2. Agarwal A, Kanekar S, Sabat S, Thamburaj K. Metronidazole-induced cerebellar toxicity. Neurol Int 2016;8:6365. 3. Roy U, Panwar A, Pandit A, Das SK, Joshi B. Clinical and neuroradiological spectrum of metronidazole induced encephalopathy: our experience and the review of literature. J Clin Diagn Res 2016;10:1–9. 4. Takada Kensuke, Maki Yoshinori, Metronidazole Induced Encephalopathy Mimicking an Acute Ischemic Stroke Event. Neurol Med Chir (Tokyo) 58, 400–403, August 3, 2018. 5. Kalpeshkumar Patel, Israel Green-Hopkins. Cerebellar ataxia following prolonged use of metronidazole: case report and literature review. International Journal of Infectious Diseases 12, 111-114, (2008). 6. Jang, Han Jin, Sook Young Sim, Jong Yun Lee, and Ji Hwan Bang. “Atypical Metronidazole-induced Encephalopathy in Anaerobic Brain Abscess.” Journal of Korean Neurosurgical Society 52 (3): 273–276, September (2012). 7. Allroggen Holger, Abbott R, Bibby K. Acute visual loss following administration of metronidazole. A case report. Departments of Neurology and Ophthalmology, Leicester, UK. Neuro-ophthalmology – 2000, Vol. 23, No. 2, pp. 89-94. 8. Kalia, et al, Brain MRI in metronidazole toxicity, Indian J Radiol Imaging. Vol 20. Issue 3, Agosto (2010). 9. Sarna Justyna, Brownell Keith, Furtado Sarah. Reversible cerebellar syndrome caused by metronidazole. Canadian Medical Association J, October 27, 2009, 181(9). 10. Patel K, Green-Hopkins I, Lu S, Tunkel AR. Cerebellar ataxia following prolonged use of metronidazole: case report and literature review. Int J Infect Dis 2008; 12 (6): 111-4. 11. S. Toumi et al. /Lésions cérébelleuses réversibles et neuropathie périphérique induites par le métronidazole/Médecine et maladies infectieuses 39 (2009) 906–908. 12. Ahmed A, Loes DJ, Bressler EL. Reversible magnetic resonance imaging findings in metronidazole-induced encephalopathy. Neurology 1995; 45 (3 Pt 1): 588-9. 13. Kapoor K, Chandra M, Nag D, et al. Evaluation of metronidazole toxicity: a prospective study. Int J Clin Pharmacol Res 1999;19:83-8. 14. Kim E, Na DG, Kim EY, et al. MR imaging of metronidazole-induced encephalopathy: lesion distribution and diffusion-weighted imaging findings. AJNR Am J Neuroradiol 2007;28:1652-8. 15. Chacko J, Pramod K, Clinical, neuroimaging and pathological features of 5-nitroimidazole-induced encephalo-neuropathy in two patients: Insights into possible pathogenesis..Neurol India 2011;59:743-7. 16. Kuriyama Akira, Jackson JL, Doi A, Kamiya T. Metronidazole-Induced Central Nervous System Toxicity: A Systematic Review. Clinical Neuropharmacology 2011;34:241–47. 17. Lee SS, Cha SH, Lee SY, Song CJ. Reversible inferior colliculus lesion in metronidazole induced encephalopathy: Magnetic resonance findings on diffusion-weighted and Fluid Attenuated Inversion 18. Recovery Imaging. J Comput Assist Tomogr 2009;33:305-8. AK Gupta, MP Agarwal, R Avasthi. Metronidazole-Induced Neurotoxicity. JAPI VOL. 51, Department of Medicine, University College of Medical Sciences and GTB Hospital, Delhi, June 2003. 19. Dong Wook Kim, Jong-Moo Park, Byung-Woo Yoon. Metronidazole-induced encephalopathy. Journal of the Neurological Sciences 224 (2004) 107–111. 20. Graves Tracey D., Condon Marie, Loucaidou Marina. Reversible metronidazole-induced cerebellar toxicity in a multiple transplant recipient. Journal of the Neurological Sciences 285 (2009) 238–240.
To cite this abstract in AMA style:
M. Teran, P. Salles. Neurological complications secondary to metronidazole: Case Report [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/neurological-complications-secondary-to-metronidazole-case-report/. Accessed March 31, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/neurological-complications-secondary-to-metronidazole-case-report/