Session Information
Date: Tuesday, September 24, 2019
Session Title: Parkinsonisms and Parkinson-Plus
Session Time: 1:45pm-3:15pm
Location: Agora 3 West, Level 3
Objective: 1): To assess Parkinson’s disease (PD) patients’ stereopsis function using better and more physiologically meaningful tools; 2): To reveal specific eye behaviors of stereoacuity impairment and whether it is feasible to use it as a biomarker of PD progression.
Background: PD patients suffer not only from motor symptoms, but also sensory visual dysfunctions. Visual and oculomotor disturbances in PD are common, including higher-level depth perception (stereopsis) and the ability to judge distance. The hampered visuospatial judgment ability in PD patients could further limit their motor navigation and cause falls and injuries. Despite its significance in early detection and progression surveillance of PD, there is still scarce scientific research on the stereopsis function in PD patients. In addition, the widely used Titmus Stereo Fly Test and Random Dot Stereogram measure stereopsis do not consider the monocular cues, nor accommodation and vergence. We see a clear need of developing a new protocol to assess stereopsis for PD patients.
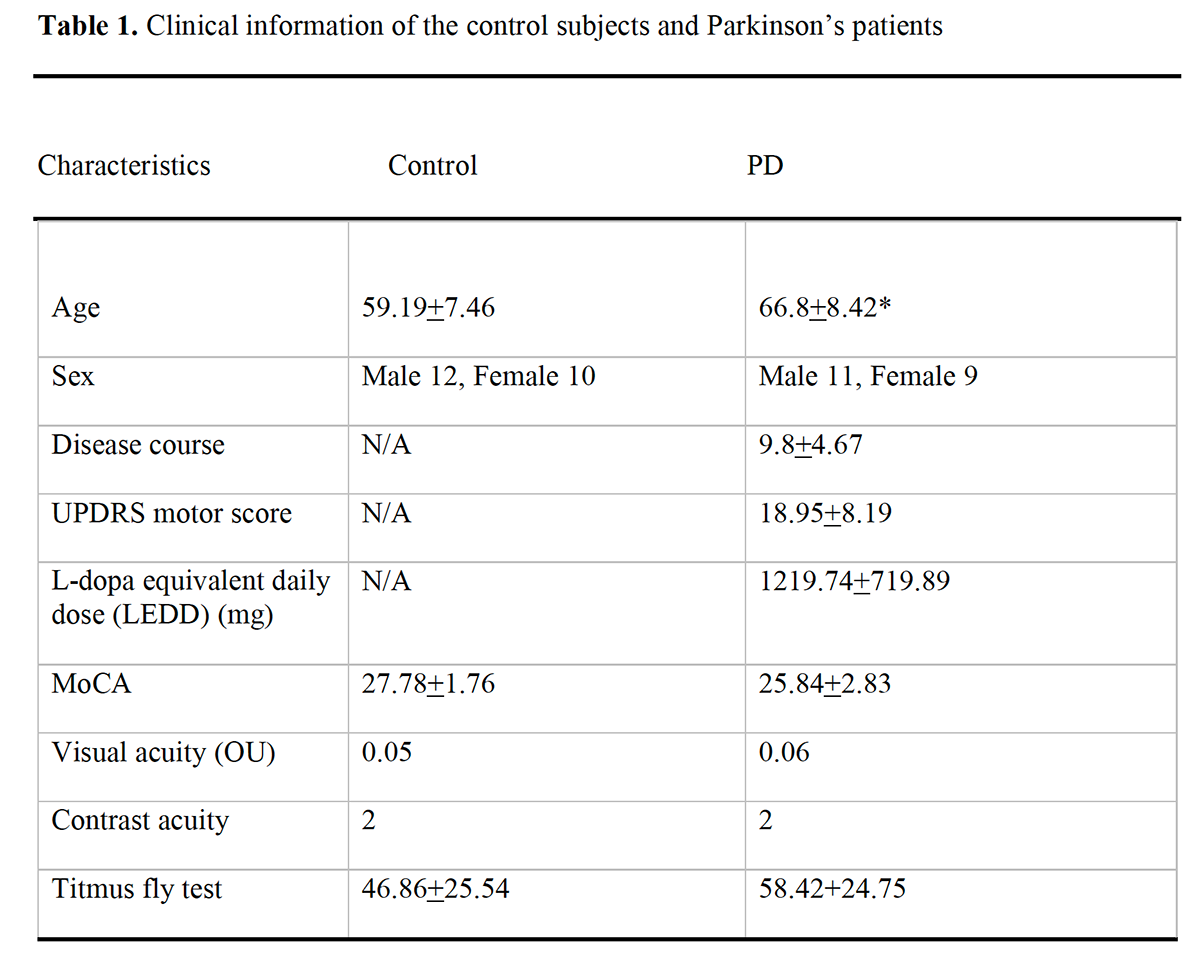
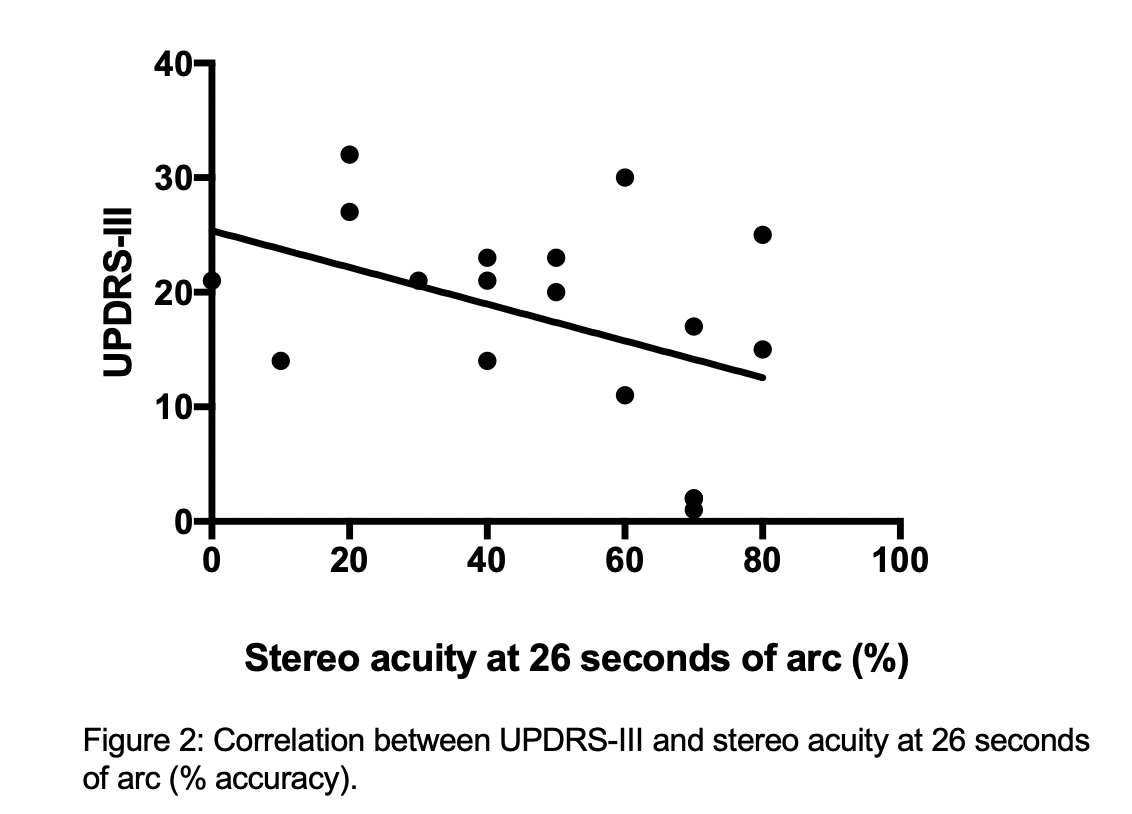
Method: Twenty PD patients, in varying disease stages (Hoehn and Yahr stage 1-4) were recruited from the Parkinson and Movement Disorders Program at the University of Alberta. They were compared to 22 sex- and age-matched control subjects (table 1). The primary outcome measures of interest were abnormalities in stereopsis and eye behavior of stereo acuity. Visual testing included visual acuity (VA), visual field, extraocular movements (EOM), contrast acuity, stereopsis with Titmus Fly and a 3D TV system. MoCA test and UPDRS were also assessed. Levodopa equivalent daily dose (LEDD) was calculated.
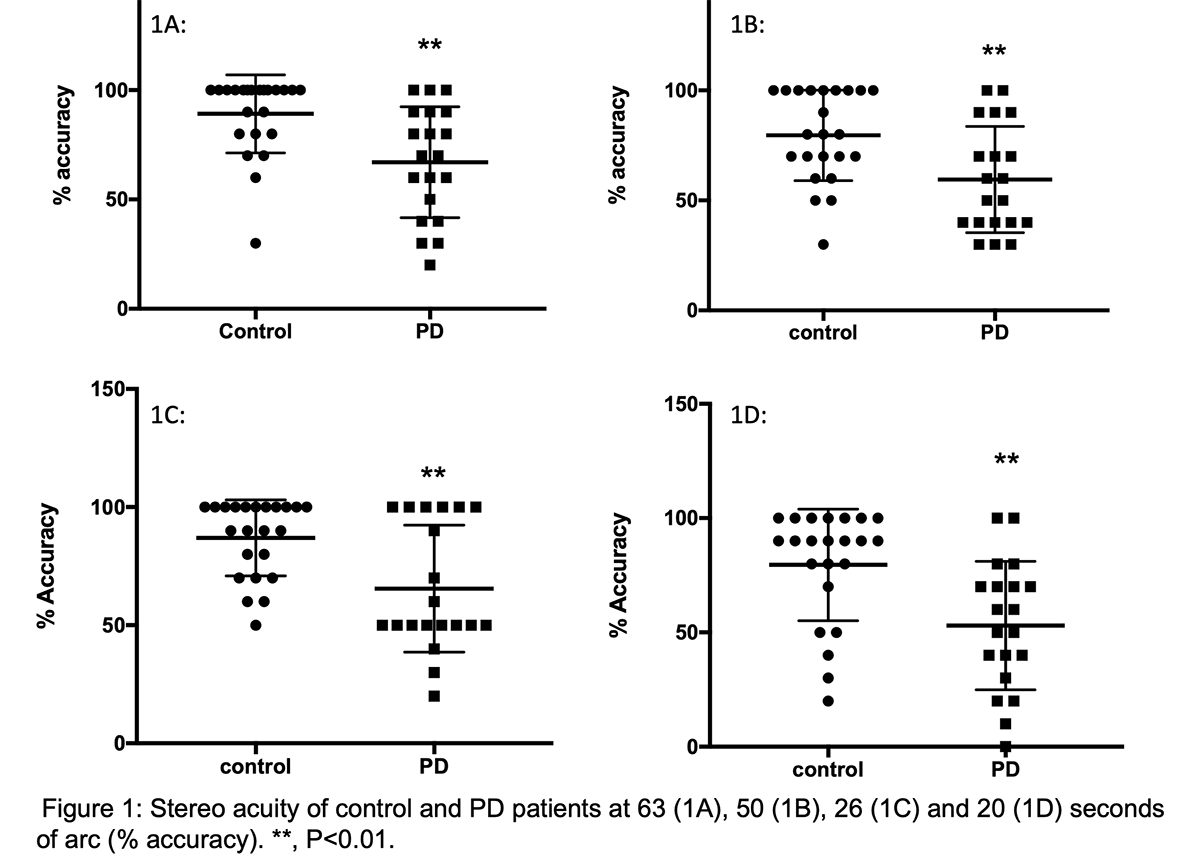
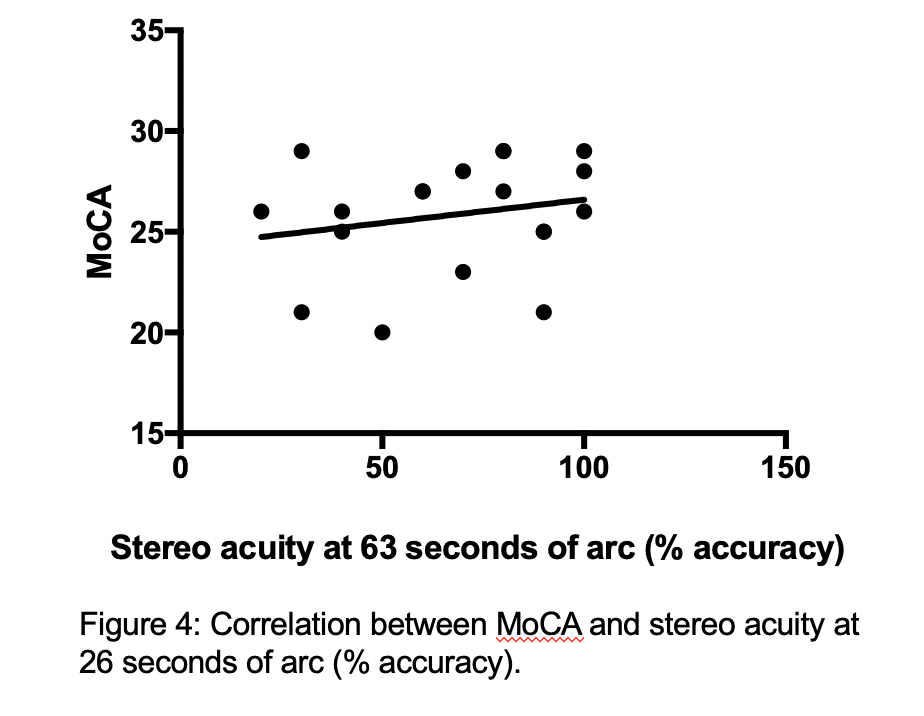
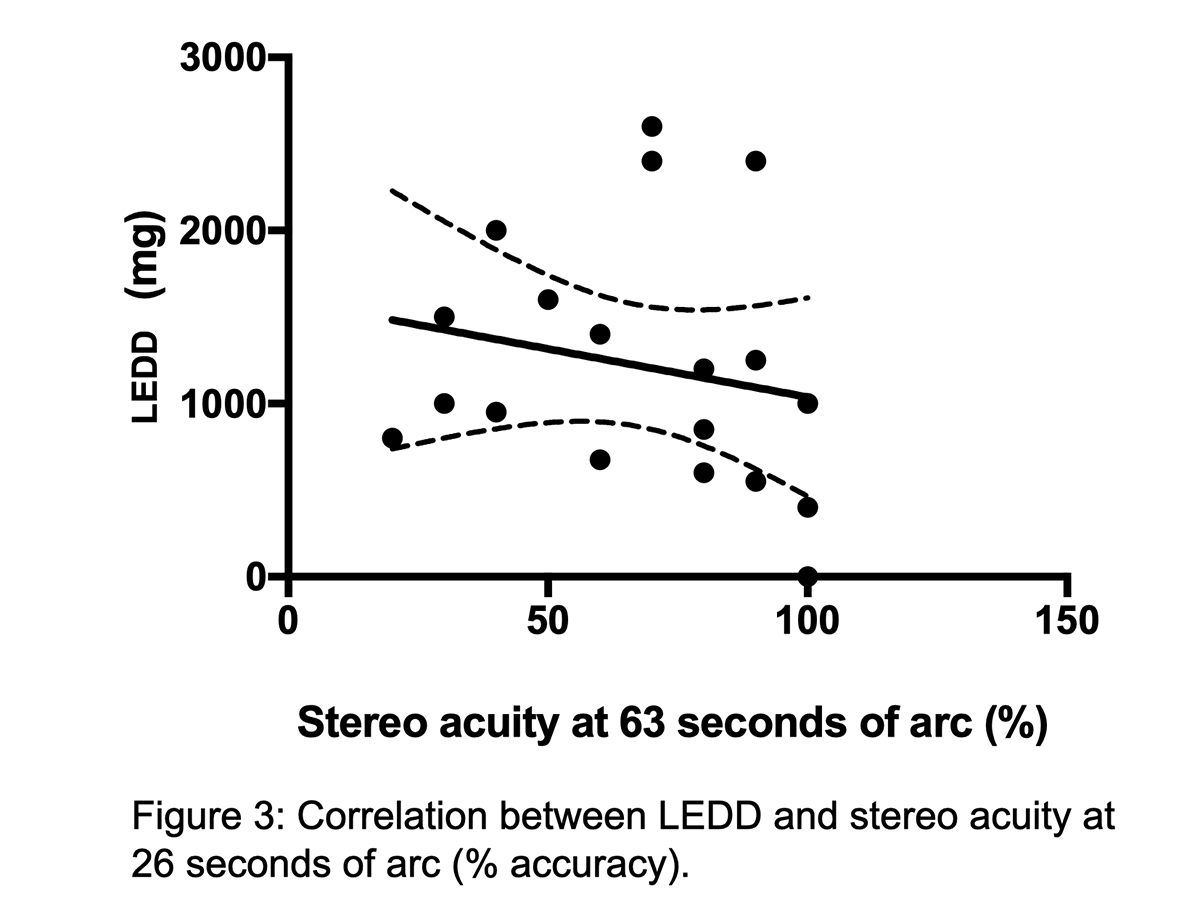
Results: There were no differences in VA, visual field or contrast acuity between the 2 groups, nor in the Titmus Stereo Fly test. Using the 3D TV system, PD patients showed a significant stereo disparity when compared to control. At 63 seconds of arc and higher acuity (figure 1), the deficit in PD was evident. The depth perception abnormalities show a trend correlating with the UPDRS-III, LEDD and MoCA (Figure 2-4, respectively).
Conclusion: Stereopsis deficit is associated with PD disease severity and cognitive status. Assessment of stereopsis using more reliable techniques may be a tool for early diagnosis and to monitor disease progression and responsiveness to treatment. Future behavioral study of gait/falls risk to correlate with stereopsis will be conducted.
To cite this abstract in AMA style:
T. Sang, J. Fatehi, E. Mostofi, B. Zheng, F. Ba. Stereopsis as a Visual Biomarker for Parkinson’s Disease [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/stereopsis-as-a-visual-biomarker-for-parkinsons-disease/. Accessed April 2, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/stereopsis-as-a-visual-biomarker-for-parkinsons-disease/