Session Information
Date: Tuesday, September 24, 2019
Session Title: Parkinsonisms and Parkinson-Plus
Session Time: 1:45pm-3:15pm
Location: Agora 3 West, Level 3
Objective: This study aims to assess the applicability of modified Vascular Parkinsonism (VP) criteria in outpatient department in a tertiary care hospital in south India.
Background: VP is not very well defined and clinically ignored entity. There is not much epidemiological data about VP from south east Asia and in the world.
Method: This is a retrospective study of the case records of Parkinsonism patients consulted in outpatient department (OPD) between May 2014 to February 2019. All outpatients, consulted to me, screened for Parkinsonism. VP was defined by Parkinsonism features ( bradykinesia, being essential criteria and/or rigidity, postural instability) and one of the vascular risk factors [ clinically diabetes mellitus (DM) ,hypertension(HTN), coronary artery disease (CAD) , cerebro-vascular accidents (CVA) and/or imaging wise small vessel disease(SVD) in MRI ] . Data collected included : demographic data, neurological findings , various vascular risk factors (DM,HTN,CAD,CVA) and MRI findings.
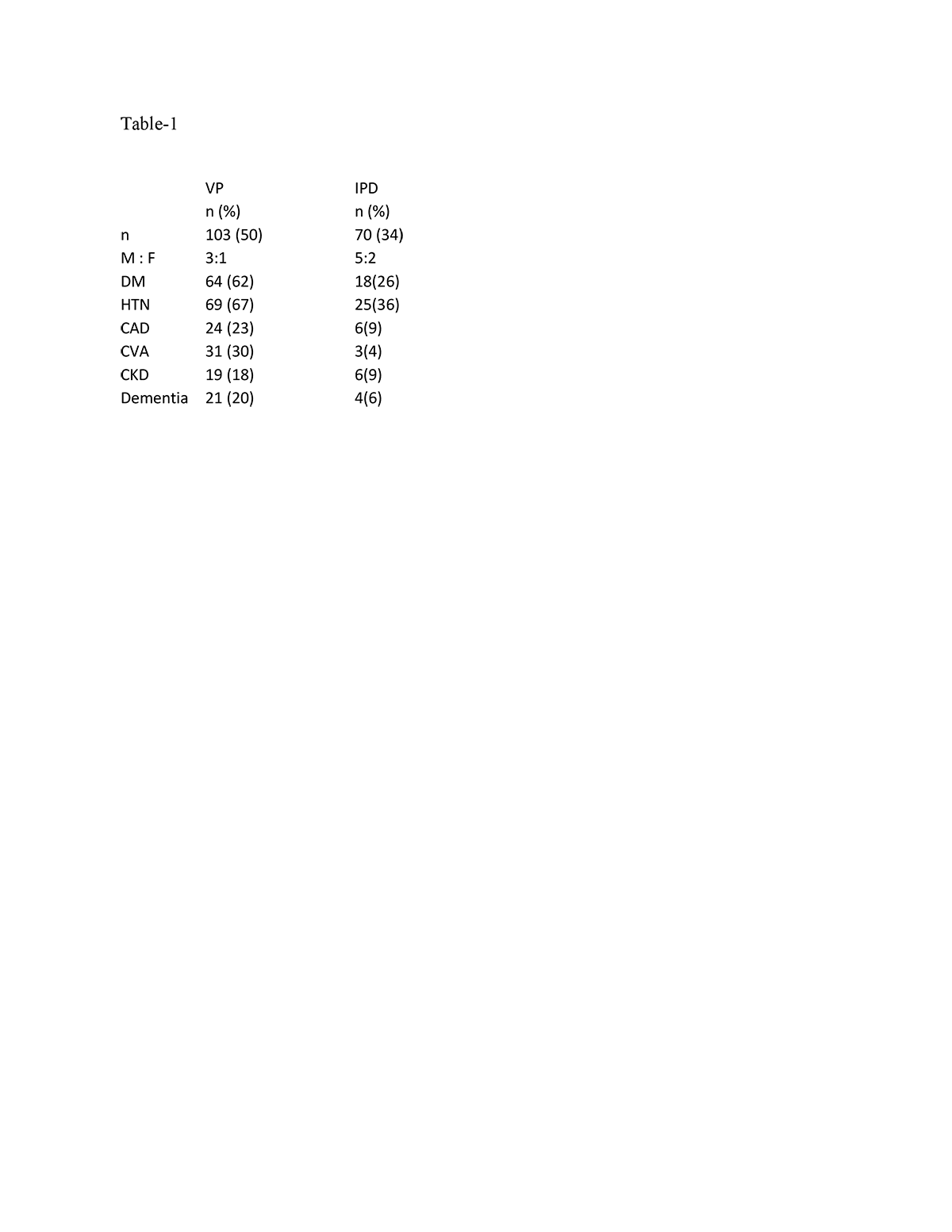
Results: During the study period of 58 months, 7959 patients with parkinsonism consulted to me in OPD. Total 204 (2.5%) patients have been diagnosed as Parkinsonism. VP was diagnosed in 103 (50.5%) patients and idiopathic Parkinson disease (IPD) was in 70 (34.3%) . Others, including PSP, MSA, NPH, Drugs induced was diagnosed in 31 (15.2%) patients. Clinical profiles of VP and IPD has been depicted in table-1. 78 (76 %) VP patients had two or more than two vascular risk factors. 20 (19%) has only single risk factor. Only 5(5%) has no risk factors and fall into possible VP and among these, 4 didn’t have imaging data. Only 13 (19%) of IPD patient has two or more than two risk factors. MRI data was available in 60 (58%) in VP patients and only in 20 (29%) IPD patients. SVD was the most common finding in 50(83%) VP patients and 9 (15 %) had vascular territory chronic infarcts. In IPD, 10 (50%) had normal MRI and 7 (35%) had SVD.
Conclusion: This study suggests that modified criteria of VP, including imaging finding and strong clinical suspicion can be applied for diagnosis of VP. This may help in giving such patients a trial of levodopa therapy, which may lead to clinical improvement of such patients.
To cite this abstract in AMA style:
S. Jaiswal. Applicability of modified definition of Vascular Parkinsonism in patients with Parkinsonism attending outpatient department: A tertiary care hospital-based study in south India [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/applicability-of-modified-definition-of-vascular-parkinsonism-in-patients-with-parkinsonism-attending-outpatient-department-a-tertiary-care-hospital-based-study-in-south-india/. Accessed April 2, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/applicability-of-modified-definition-of-vascular-parkinsonism-in-patients-with-parkinsonism-attending-outpatient-department-a-tertiary-care-hospital-based-study-in-south-india/