Session Information
Date: Monday, September 23, 2019
Session Title: Psychiatric Manifestations
Session Time: 1:45pm-3:15pm
Location: Les Muses Terrace, Level 3
Objective: Identify, in Mexican patients with PD, the prevalence of SD as well as its impact on cognitive and motor impairment.
Background: SD refers to the presence of discomforts that the person perceives related to different bodily dysfunctions but do not have an organic or physiological cause. Although the incidence of SD is greater in PD and there are some studies that show an association between SD and cognitive impairment in these patients; The impact of SD on motor disability has been little addressed. The SCL-90R is a validated tool for the assessment of psychopathological symptoms. It is composed of nine symptom dimensions. Each item of each dimension in the SCL-90R is measured in terms of how much the symptom is bothering the participant. it is scored in the scale ranging from 0=not at all to 4=extremely. The score of each dimension is the mean of all items of that dimension. Patients without the symptom scores <1; mild symptoms 1 to 2; moderate-severe symptoms >2. We considered the SD dimension, which consists of 12 items.
Method: Observational, analytical cross-sectional study, where SD subscale of SCL-90R scale was performed in 100 patients with PD, as well as MOCA test and MDS-UPDRS. Patients were evaluated in the movement disorders clinic of the National Institute of Neurology “Manuel Velasco Suárez” in a period of 2 months.
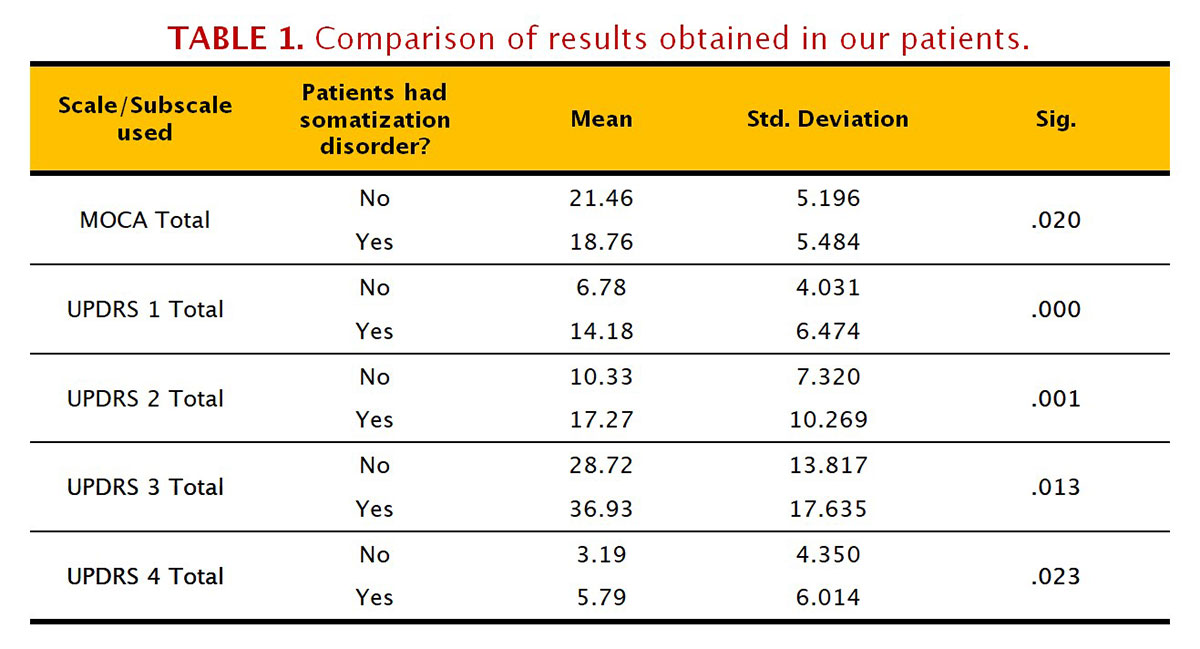
Results: We include 100 patients; men (53.1%) and women (46.9%) with an average age of 64.26 years ± 12.4. Within our group of patients, we observed that 42.7% had symptoms of SD (34.4% with mild symptoms and 8.3% with moderate to severe symptoms). MOCA: SD (mean score(M) = 18.76); without SD (M = 21.46); (p = 0.02). UPDRS1: SD (M = 14.18); without SD (M = 6.78); (p = 0.000). UPDRS2: SD (mean = 17.27); without SD (M = 10.33); (p = 0.001). UPDRS3: SD (M = 36.93); without SD (M = 28.72); (p = 0.013). UPDRS4: SD (M = 5.79); without SD (M = 3.19); (p = 0.023).
Conclusion: We could confirm the high prevalence of SD in our population, as well as a significant difference in all the areas evaluated when comparing both groups, that is a greater cognitive deterioration and a worse performance in all the sections of the MDS-UPDRS in patients with a SD. Subsequent studies considering the impact on the treatment and prognosis of these patients may be beneficial.
References: 1. Siri, C; Cilia, R; Gaspari, D; Villa, F; Goldwurm, S; Marco, C; Pezzoli, G; Antonini,A. Psychiatric Symptoms in Parkinson´s disease assessed with the SCL-90 R self-reported questionnaire. Neurol Sci, (2010) 31:35–40. 2. Carrozino, D; Morberg, B; Siri, C; Pezzoli, G; Bech, P. Evaluating psychiatric symptoms in Parkinson´s Disease by a clinimetric analysis of the Hopkins Symptom Checklist (SCL-90-R). Progress in Neuropsychopharmacology & Biological Psychiatry, (2017). 3.Onofrj, M; Bonanni, L; Manzoli, L; Thomas, A. Cohort study on somatoform disorders in Parkinson disease and dementia with Lewy bodies. Neurology (2010);74: 1598–606.
To cite this abstract in AMA style:
M. Rodriguez-Violante, A. Cervantes-Arriaga, A. Polo-Morales, A. Alcocer-Salas. Somatization disorder (SD) and Parkinson’s Disease (PD) in Mexican population [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/somatization-disorder-sd-and-parkinsons-disease-pd-in-mexican-population/. Accessed April 3, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/somatization-disorder-sd-and-parkinsons-disease-pd-in-mexican-population/