Session Information
Date: Monday, September 23, 2019
Session Title: Neuropharmacology
Session Time: 1:45pm-3:15pm
Location: Les Muses Terrace, Level 3
Objective: To compare Parkinson’s disease (PD) treatment practices by movement disorder (MD) specialists across a decade, and to determine the factors that influence drug choice in newly diagnosed drug-naïve PD patients in Singapore.
Background: Treatment in PD is symptomatic and guided largely by best clinical practices, with evidence for a levodopa-sparing strategy (LDS) still evolving. Furthermore, potential adverse drug events (ADE) identified during postmarketing surveillance continue to influence drug choice. Few long-term longitudinal data exist on anti-parkinsonian drug (APD) prescribing patterns.
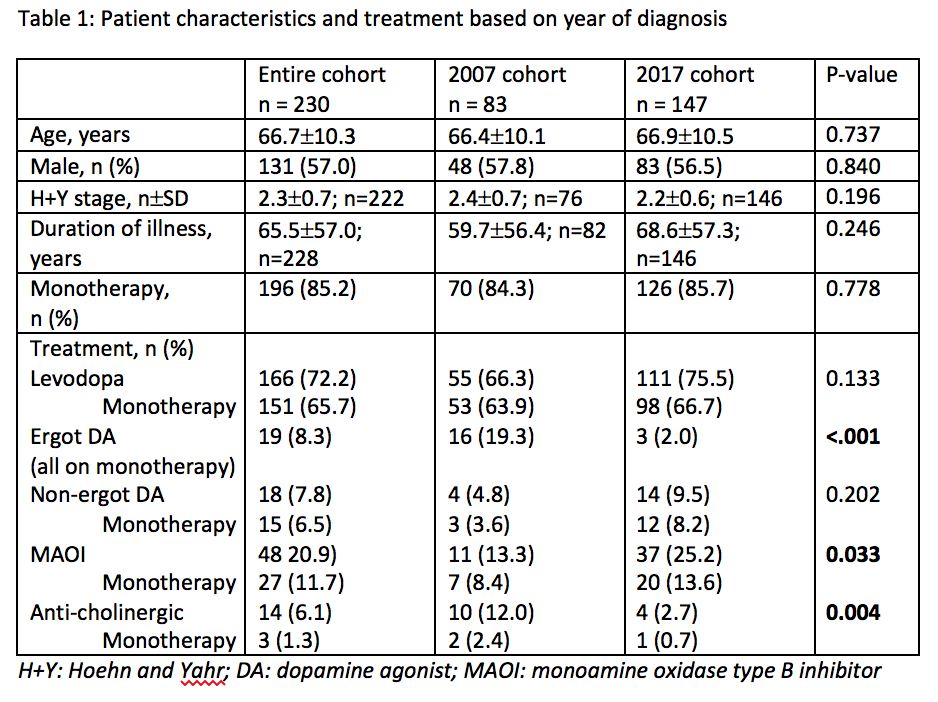
Method: This cross-sectional analysis included drug-naïve PD patients, diagnosed in the years 2007 and 2017, and seen within 1 year of diagnosis by a MD specialist at a large tertiary referral centre, who were started on medications within the first two clinic visits. Discontinuation of treatment was determined at two subsequent follow-up visits occurring within 2 years from first visit. Demographic, clinical and prescription data were extracted from our centre’s movement disorder database.
Results: From 2007 to 2017, the use of ergot dopamine agonists and anti-cholinergics decreased (19.3% to 2.0%, p<.001 and 12.0% to 2.7%, p=.004 respectively) while monoamine oxidase B inhibitor (MAOI) use increased (13.3% to 25.2%, p=.033). Use of LDS decreased non-significantly from 33.7% to 24.5%. [table 1] Compared to levodopa users, patients on LDS were younger (57.5±8.1 vs 70.3±8.8 years, p<.001) and had milder disease (H+Y stage 1.9±0.5 vs 2.4±0.7, p<.001). Age >=70 (aOR 11.9; 4.5-31.5) and H+Y stage >2 (aOR 3.4; 1.5-7.7) were independent factors for levodopa use, even after subgroup analysis by year of diagnosis. Non-levodopa prescriptions were more likely to be discontinued compared to levodopa (13/92 (14.1%) vs 6/149 (4.0%), p=.005), with MAOI accounting for 8/13.
Conclusion: APD prescribing patterns in PD have changed significantly through the last decade, possibly influenced by emerging evidence and ADE reports. Key guiding factors of choosing drugs based on patient’s age and disease severity remained consistent across the years. It is important that international and national guidelines for drug prescribing in PD be updated and consistent throughout different socioeconomic settings to optimize care.
To cite this abstract in AMA style:
S. Neo, A. Wong, HL. Ng, W. Li, KY. Tay, WL. Au, L. Tan. Evolution of anti-parkinsonian drug prescribing patterns in Parkinson’s disease [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/evolution-of-anti-parkinsonian-drug-prescribing-patterns-in-parkinsons-disease/. Accessed January 6, 2026.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/evolution-of-anti-parkinsonian-drug-prescribing-patterns-in-parkinsons-disease/