Session Information
Date: Monday, October 8, 2018
Session Title: Parkinson's Disease: Non-Motor Symptoms
Session Time: 1:15pm-2:45pm
Location: Hall 3FG
Objective: To develop and validate a novel questionnaire to assess various aspects related to problems experienced by PD patients when turning in or getting out of bed during the night.
Background: Nocturnal hypokinesia (NH) is a decreased ability to perform sufficient axial rotation and/or trunk flexion to turn in or get out of bed as a result of limb and axial muscle incoordination, and affects up to 70% of patients with PD. To date, there are no validated questionnaires, specifically developed for assessing NH in PD patients.
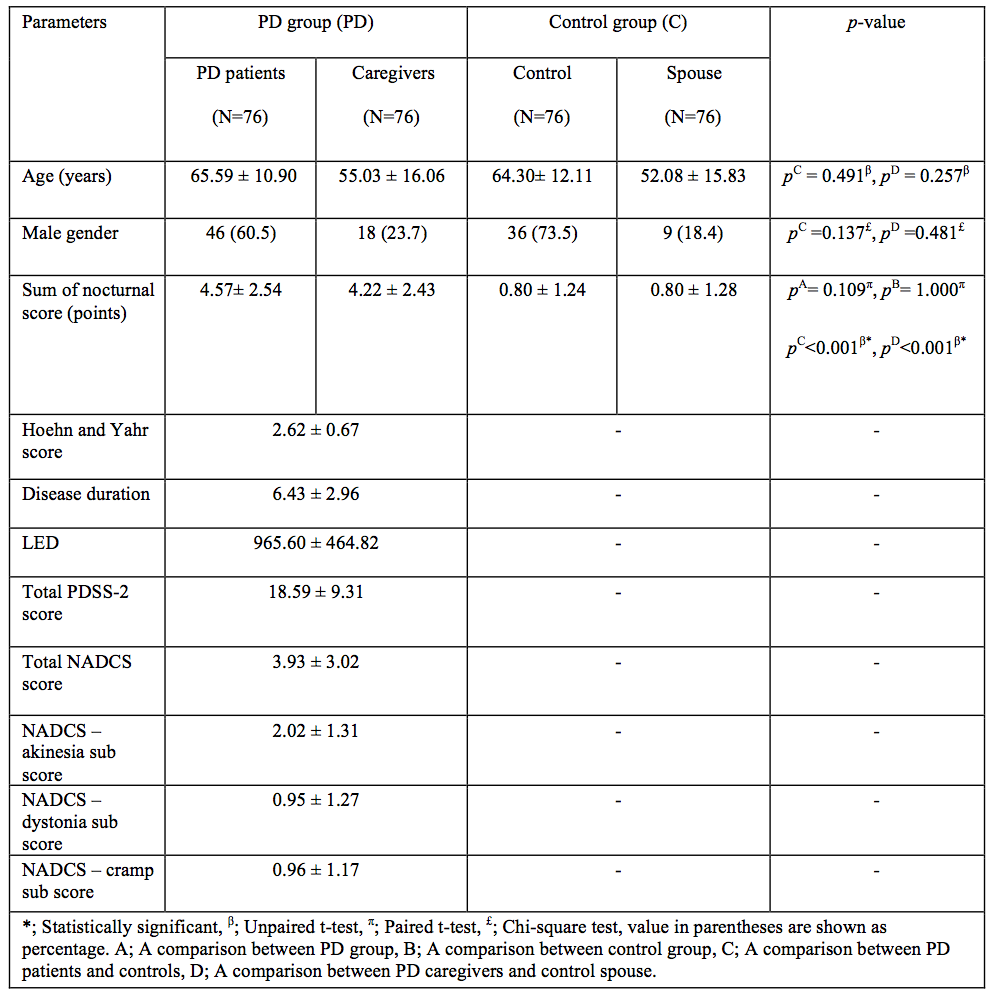
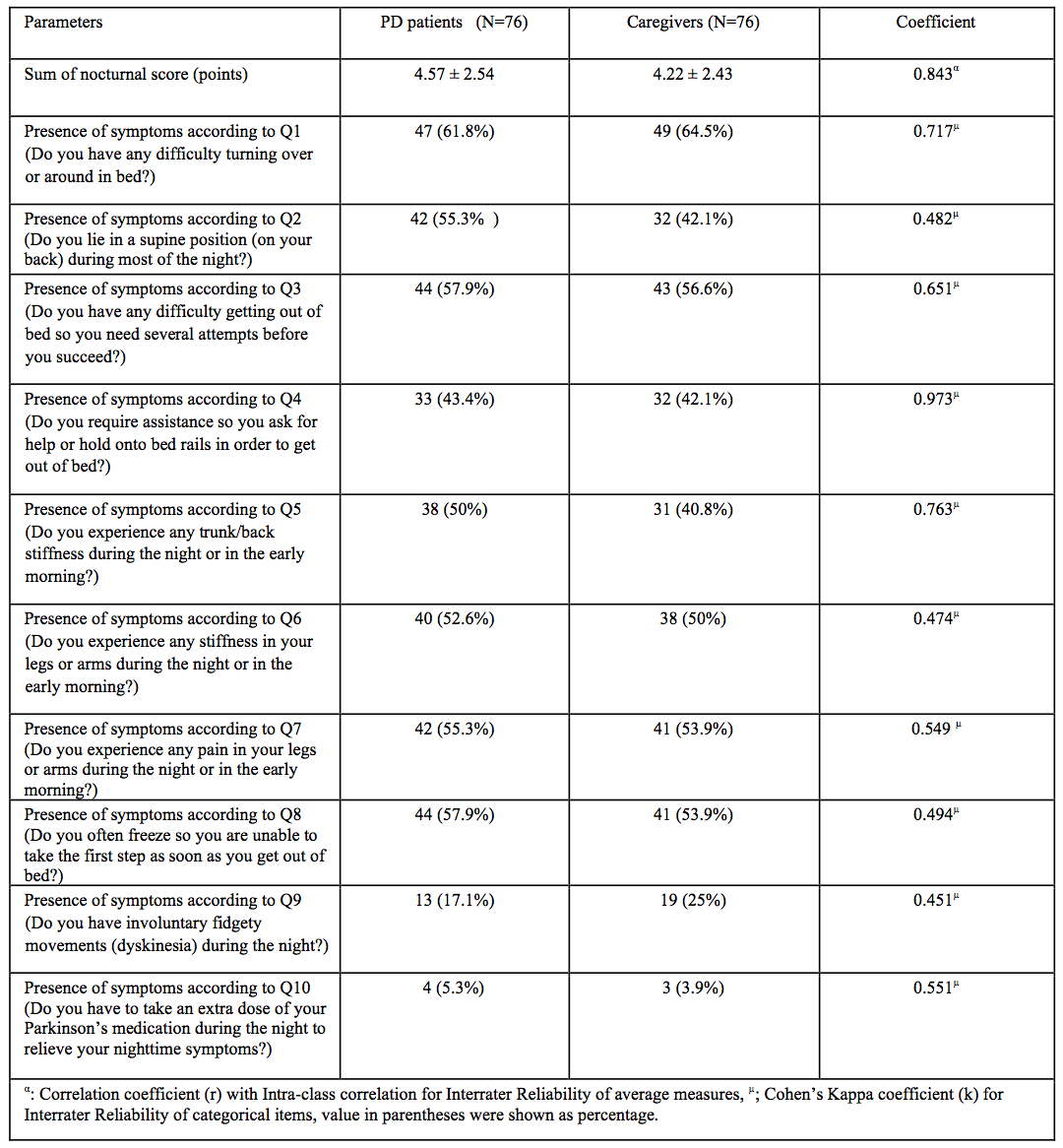
Methods: The NH questionnaire (NHQ) consists of 10 items, which are completed independently by patients and their spouses (Table 1). For validation, 76 PD patient pairs, recruited from specialist movement disorder clinic, completed the questionnaire and agreement levels, content validity, and internal consistency were assessed (Table 2). Another set of 76 healthy couples served as controls. Correlations were performed between the NHQ and Modified Parkinson’s Disease Sleep Scale (PDSS-2). A random sample of 25 patient pairs were also assessed with objective night-time monitoring to provide additional correlations.
Results: Patients and caregiver-based scores were compared and agreement has been achieved to determine the reliability of spouse evaluation of patient’s NH symptoms (Cohen Kappa’s coefficient: 0.45-0.97). Comprehension of items was tested for content validity with an IOC index of above 0.6 for all items. High internal consistency was confirmed by KR-20 coefficient of 0.737 and 0.694 for both patients and spouses respectively. There was no significant difference for the mean total score from PD patients (4.57 + 2.54), compared to the spouses (4.22 + 2.43, p=0.109). However, mean NHQ scores obtained from PD patients and their spouses were significantly higher than healthy couples accordingly (p<0.001). Moderate and significant correlations were found between the NHQ and PDSS-2 (0.33, p=0.004), as well as objective monitoring as demonstrated by number and degree of axial rotations (-0.41, p=0.04; -0.44, p=0.02 respectively).
Conclusions: In this study, NHQ is found to be a reliable instrument to identify symptoms related to NH in PD. Strong patient-spousal agreement supports the use of proxy evaluation by spouses when patient’s information is unobtainable.
References: 1. Sringean J, Taechalertpaisarn P, Thanawattano C, Bhidayasiri R. How well do Parkinson’s disease patients turn in bed? Quantitative analysis of nocturnal hypokinesia using multisite inertial wearable sensors. Parkinsonism Relat Disord. 2016;23:10-16. 2. Bhidayasiri R, Trenkwalder C. Getting a good night sleep? The importance of recognizing and treating nocturnal hypokinesia in Parkinson’s disease. Parkinsonism Relat Disord. 2018 doi: 10.1016/j.parkreldis.2018.01.008. [Epub ahead of print].
To cite this abstract in AMA style:
R. Bhidayasiri, O. Jitkritsadakul, J. Sringean, P. Martinez-Martin, C. Anan, N. Kantachadvanich, R. Chaudhuri, N. Hattori. Validation of a patient/caregiver questionnaire to evaluate nocturnal hypokinesia in Parkinson’s disease [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/validation-of-a-patient-caregiver-questionnaire-to-evaluate-nocturnal-hypokinesia-in-parkinsons-disease/. Accessed November 27, 2025.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/validation-of-a-patient-caregiver-questionnaire-to-evaluate-nocturnal-hypokinesia-in-parkinsons-disease/