Session Information
Date: Monday, October 8, 2018
Session Title: Parkinson's Disease: Non-Motor Symptoms
Session Time: 1:15pm-2:45pm
Location: Hall 3FG
Objective: Non motor symptoms (NMS) in idiopathic Parkinson’s disease (PD) are well studied and has an effect on quality of life in PD. NMS in Atypical Parkinsonism (AP) are not conventional and need more studies. The present study was planned to evaluate Non motor symptoms in patients with AP.
Background: AP are a group of neurodegenerative disorders characterized by parkinsonism along with early postural instability, cognitive decline, autonomic failure, apraxia, pyramidal, cerebellar signs, etc. There are various NMS in both AP and PD but unlike PD relatively little literature is available about quantification of all NMS in AP. Also NMS in AP has not been studied in Indian patients. To evaluate NMS in Indian patients, this study was planned, and patients with PD, Multiple System Atrophy (MSA) and Progressive Supranuclear Palsy (PSP) were enrolled.
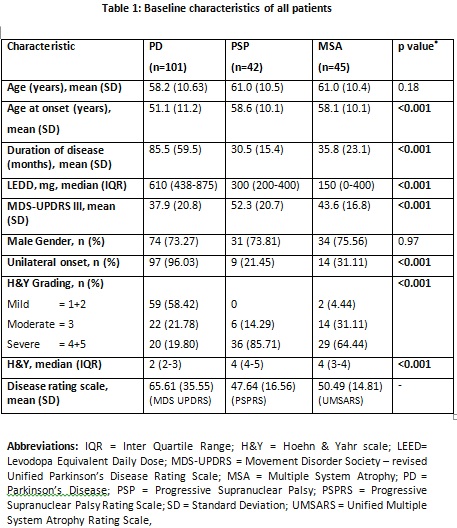
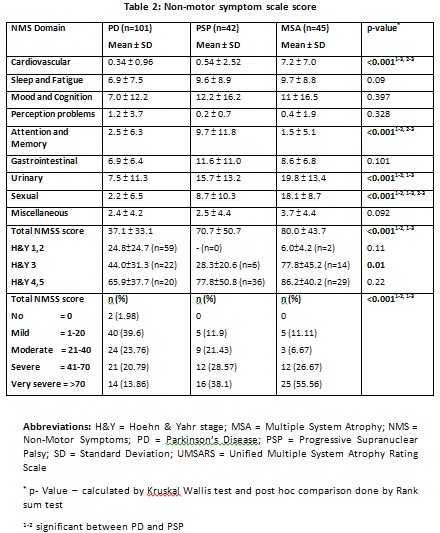
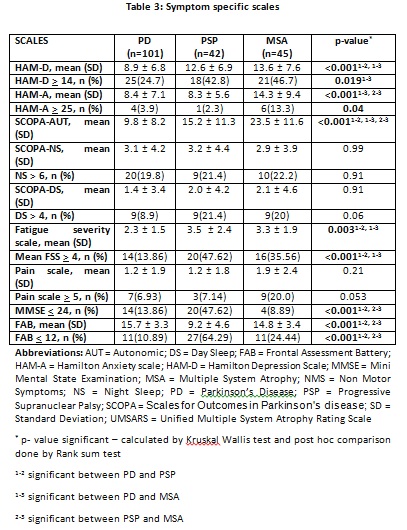
Methods: This single center, cross-sectional study enrolled 188 patients (101 PD, 42 probable/possible PSP and 45 probable/possible MSA) from a movement disorder clinic of a tertiary care teaching hospital. Various scales were used to assess disease severity (Hoehn & Yahr staging, H&Y) , motor disability (Movement Disorder Society – revised Unified Parkinson’s Disease Rating Scale, MDS-UPDRS part III), non-motor symptoms (Non Motor Symptom Scale, NMSS), parkinsonism rating scales {(MDS-UPDRS), UMSARS (Unified Multiple System Atrophy Rating Scale) & PSPRS (Progressive Supranuclear Palsy Rating scale)}, depression and anxiety (Hamilton scales: HAMD, HAMA), Sleep (Scale for Outcomes in Parkinson’s disease, SCOPA-Sleep scale), autonomic dysfunction (SCOPA-AUT scale), pain (Nominal scale), fatigue (Fatigue severity scale, FSS) and cognition (Mini-Mental State Examination, MMSE and Frontal Assessment Battery,FAB scales).
Results: The mean age of patients was comparable with male dominance (73%, p > 0.05). Patients with PD were younger at onset with longer duration of disease (p<0.001). Disease severity and motor disability were worse in Atypical Parkinsonism (PSP>MSA) (p<0.001). The mean NMSS score was 37.1 ± 33.1, 70.7 ± 50.7 and 80.0 ± 43.7 in PD, PSP and MSA, respectively (p<0.001). Median number of symptoms (IQR) reported was 7 (4-10), 10 (5.25– 13.75) and 11 (9-15) by PD, PSP and MSA, respectively (p=0.001). MSA had higher scores for cardiovascular and sexual domain, PSP had higher scores for attention/memory domain and PD had significantly lower scores for urinary domain on post hoc comparison (p<0.001).
Conclusions: This study comparing NMS in AP as compared to PD shows that NMS are worse among AP. The burden of NMS was worse in MSA > PSP > PD. These disorders could be recognised through prominent cardiovascular and sexual symptoms in MSA and attention/memory symptoms in PSP.
To cite this abstract in AMA style:
V. Kataria, V. Goyal. Non motor symptoms in parkinsonism: A cross sectional study [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/non-motor-symptoms-in-parkinsonism-a-cross-sectional-study/. Accessed October 22, 2025.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/non-motor-symptoms-in-parkinsonism-a-cross-sectional-study/