Session Information
Date: Monday, October 8, 2018
Session Title: Parkinson's Disease: Non-Motor Symptoms
Session Time: 1:15pm-2:45pm
Location: Hall 3FG
Objective: To investigate the relationship between α synucleinopathy-induced enteric neuropathy and gastrointestinal dysfunction in A53T mice.
Background: Approximately 80-90% of PD patients suffer from GI symptoms including dysphagia (swallowing difficulty), gastroparesis (slowed stomach emptying) and chronic constipation. Importantly, these GI symptoms often precede the onset of motor deficits by decades (1). GI function is primarily controlled by the enteric nervous system (ENS), a subdivision of the autonomic nervous system, and its central nervous system (CNS) connections. Beginning in the oesophagus and extending down to the anus, the ENS is embedded in the lining of the GI tract and interacts with the CNS through parasympathetic (vagus and pelvic nerves) and sympathetic (prevertebral ganglia) connections to regulate contraction, relaxation, secretion and absorption throughout the GI tract. It is well established that changes at the level of the ENS have functional GI consequence (2). Whilst the identification of abnormalities in the ENS of PD sufferers was discovered over 30 years ago and these changes have been acknowledged as a key contributor in the manifestation of PD-induced GI dysfunction, the relationship between α synuclein aggregation, ENS deterioration and the onset of GI dysfunction remains unclear.
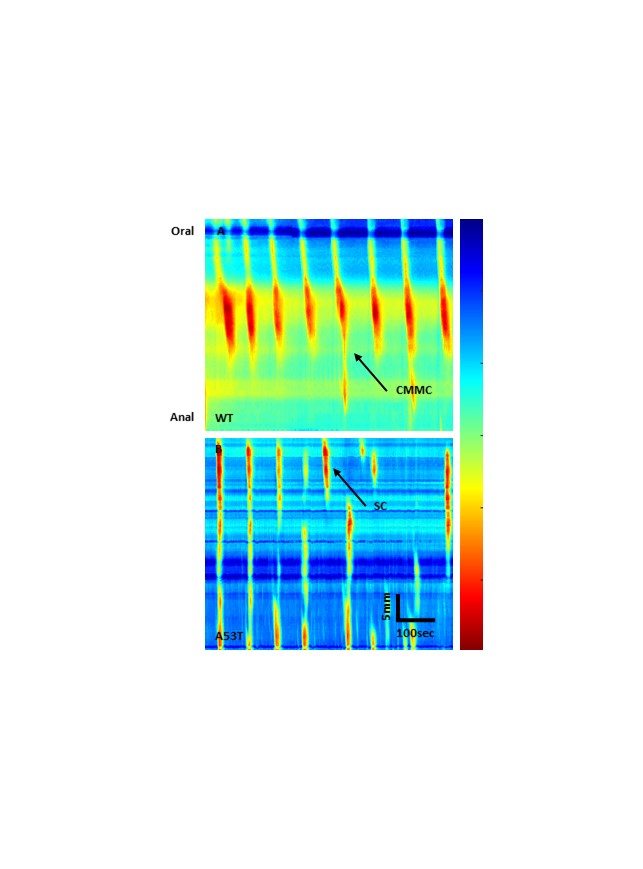
Methods: Male and female human α synuclein overexpressing transgenic (A53T) mice and WT littermate controls aged 7 months were euthanised by cervical dislocation and the entire colon was removed. Colons were arranged horizontally in organ-bath chambers and the contractile activity of each colon was video recorded and used to construct spatiotemporal maps using in-house edge detection software. Separate segments of colon tissue were loaded with a high-affinity Ca2+ indicator, Fluo-4 and optically probed via in situ calcium imaging to evaluate electrically excitable in the ENS.
Results: α-synuclein overexpressing transgenic mice (A53T) had significantly reduced colonic motor activity compared to WT mice, this loss was primarily due to a reduction in the number and proportion of short propagating contractions. Changes in colonic motor activity demonstrated in A53T mice corresponded with altered Ca2+ signalling at the level of the myenteric plexus.
Conclusions: Our research investigating motor patterns in isolated colon indicate that GI dysfunction in A53T human α synuclein overexpressing transgenic mice is intrinsically mediated by the ENS.
References: 1. Fasano A, Visanji NP, Liu LW, Lang AE, Pfeiffer RF. Gastrointestinal dysfunction in Parkinson’s disease. The Lancet Neurology. 2015:625-39. 2. Wood JD. Enteric Nervous System: Neuropathic Gastrointestinal Motility. Digestive diseases and sciences. 2016:1-14.
To cite this abstract in AMA style:
R. McQuade, P. Rajasekhar, S. Diwakarla, R. Constable, D. Poole, J. Berger, D. Finkelstein, J. Furness. Gastrointestinal Symptoms and Enteric Nerve Dysfunction in A53T Mice [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/gastrointestinal-symptoms-and-enteric-nerve-dysfunction-in-a53t-mice/. Accessed December 23, 2025.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/gastrointestinal-symptoms-and-enteric-nerve-dysfunction-in-a53t-mice/