Session Information
Date: Monday, October 8, 2018
Session Title: Parkinson's Disease: Non-Motor Symptoms
Session Time: 1:15pm-2:45pm
Location: Hall 3FG
Objective: To test the hypothesis that constipation and gastrointestinal (GI) dysautonomia may be correlated with nigrostriatal dopaminergic (DA) dysfunction in PD.
Background: Constipation is a prodromal feature of PD and the GI tract is implicated in the pathogenesis of PD. Autopsy evidence supports nigral degeneration as a correlate of late-life constipation (Petrovitch et al., 2009), but no studies have demonstrated ante-mortem relationships between nigrostriatal dysfunction and GI dysautonomia in PD. However, it was recently demonstrated in rodents that nigral projections regulate gastrointestinal motility via DA receptors on neurons in the dorsal vagal complex (Anselmi et al., 2017).
Methods: The Scale for Outcomes in Parkinson’s disease for Autonomic Symptoms (SCOPA-AUT) assesses dysautonomia in the multi-center Parkinson’s Progression Marker Initiative (PPMI). We used linear mixed-effects (LME) models and reliable change indices (RCIs) to examine longitudinal associations between dysautonomia and dopamine transporter (DAT) striatal binding ratios (SBRs) measured by single-photon emission computerized tomography (SPECT) in PPMI participants over four years (n=397 at baseline).
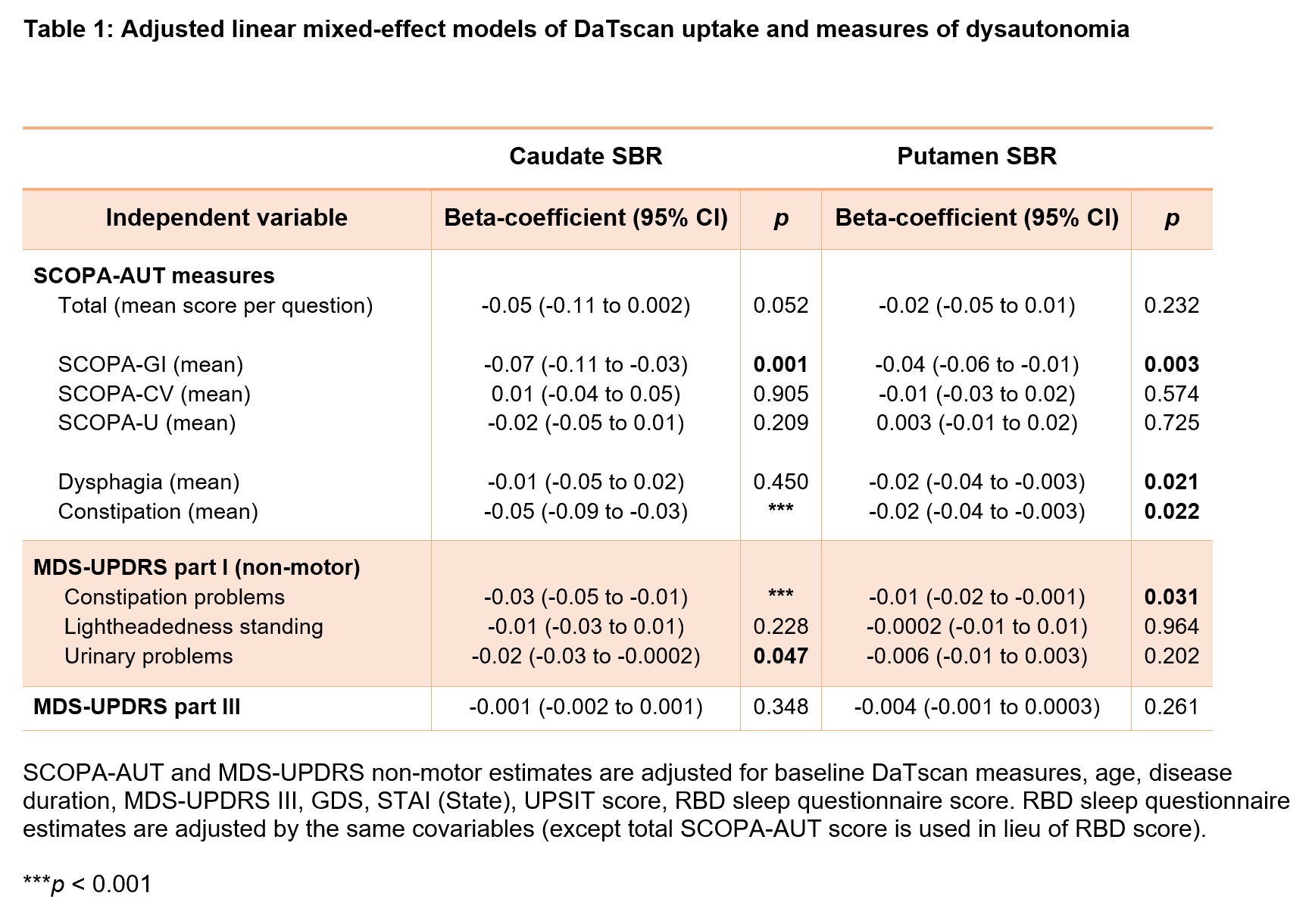
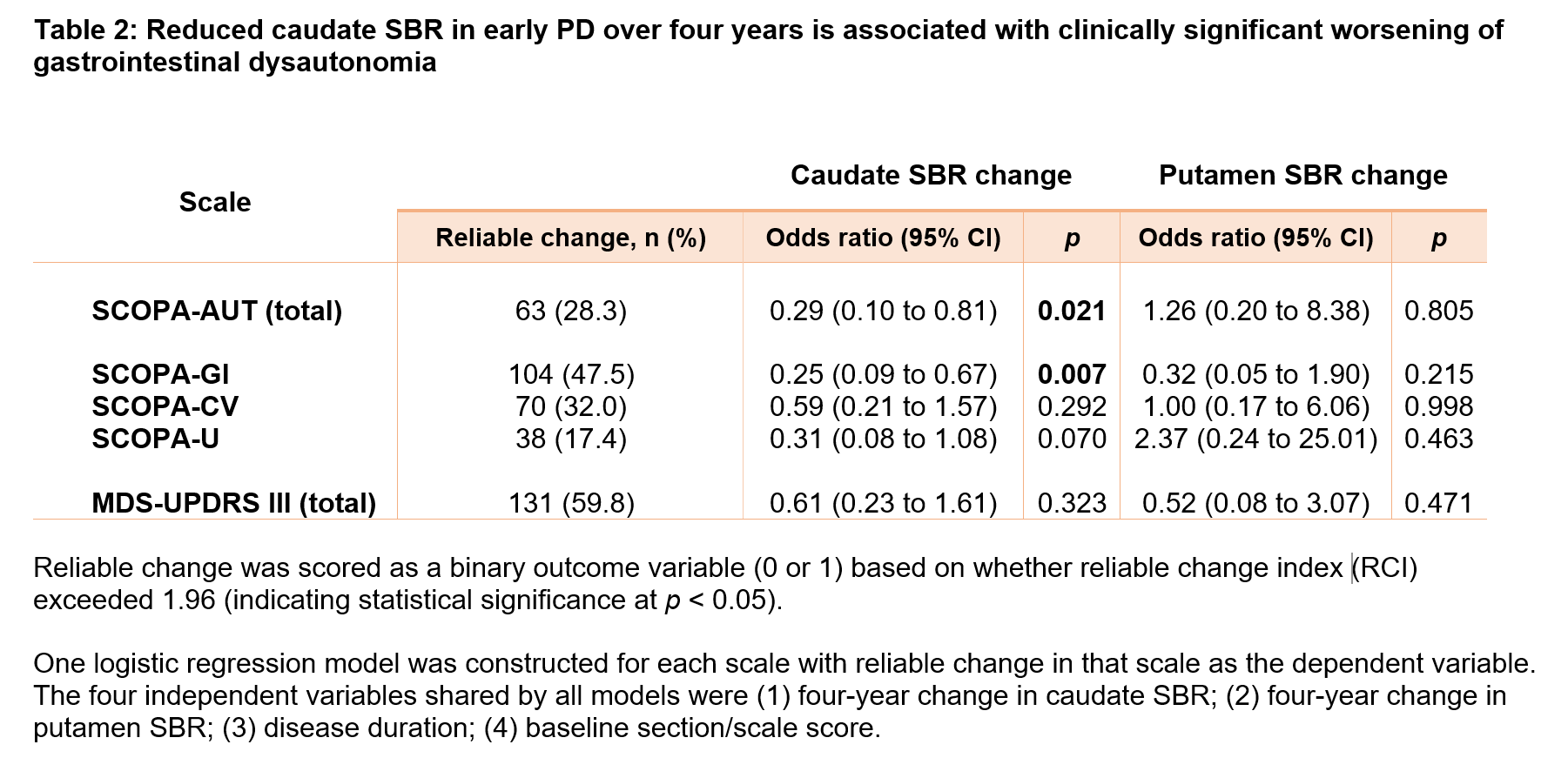
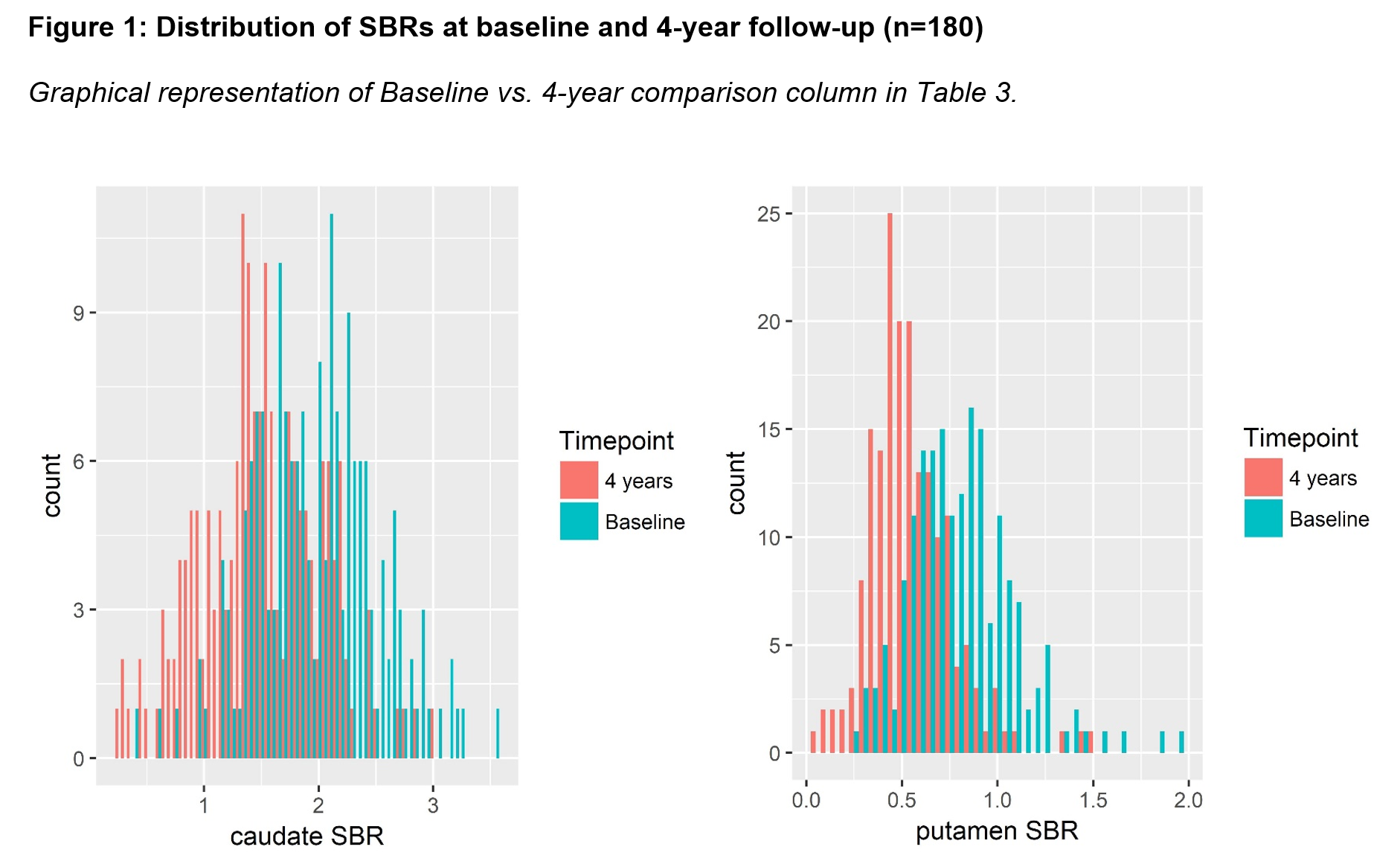
Results: Adjusted LME models of longitudinal data [table1] showed that constipation—but not orthostatic hypotension or urinary dysfunction—was associated with reduced SBR in both caudate (P<0.001) and putamen (P=0.022). In both regions, SBR reductions between baseline and 4-year follow-up were significant and measurable (P < 0.0001), with larger decline and variances in the caudate nucleus [figure1]. Logistic regression adjusting for disease duration and baseline SCOPA-GI score showed that 4-year change in caudate—but not putaminal —SBR was significantly associated with RCI-indicated progression of GI dysautonomia (P=0.007), but not other types of dysautonomia [table2]. The association remained after adjusting for the use of medications or supplements to control constipation. Consistent with prior PPMI reports, motor impairment progression was not associated with SBR reduction.
Conclusions: GI dysautonomia correlates with reduced striatal DAT availability in PD and constipation may be most closely associated with caudate-DAT reductions. Worsening GI dysautonomia may accompany advancing nigral degeneration or changes in nigrostriatal dopamine function.
References: Anselmi L, Toti L, Bove C, Hampton J, Travagli RA. A Nigro-Vagal Pathway Controls Gastric Motility and is Affected in a Rat Model of Parkinsonism. Gastroenterology 2017: 36138–3. Petrovitch H, Abbott RD, Ross GW, Nelson J, Masaki KH, Tanner CM, et al. Bowel movement frequency in late-life and substantia nigra neuron density at death. Mov. Disord. 2009; 24: 371–376.
To cite this abstract in AMA style:
J. Hinkle, K. Perepezko, K. Mills, Z. Mari, A. Butala, T. Dawson, A. Pantelyat, L. Rosenthal, G. Pontone. Striatal dopamine transporter availability changes reflect gastrointestinal dysautonomia severity in early Parkinson’s disease [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/striatal-dopamine-transporter-availability-changes-reflect-gastrointestinal-dysautonomia-severity-in-early-parkinsons-disease/. Accessed April 1, 2025.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/striatal-dopamine-transporter-availability-changes-reflect-gastrointestinal-dysautonomia-severity-in-early-parkinsons-disease/