Session Information
Date: Sunday, October 7, 2018
Session Title: Parkinsonism, MSA, PSP (Secondary and Parkinsonism-Plus)
Session Time: 1:45pm-3:15pm
Location: Hall 3FG
Objective: Our study aims to identify diagnostic markers of atypical parkinsonian disorders that offer novel insights into these conditions. In particular, we wish to use fluid biomarkers to explore the role of inflammation.
Background: The high degree of clinical overlap between atypical parkinsonian syndromes (APS) and PD makes diagnosis challenging and so pathological diagnosis remains the gold standard. In recent times, neurofilament light chain (NFL), a marker of axonal degeneration, has been shown to reliably differentiate APS from PD and healthy controls in both CSF (1) and plasma (2). However, NFL does not differentiate between PSP, CBS and MSA and offers little insight into dysfunctional biological pathways that may lead to neurodegeneration.
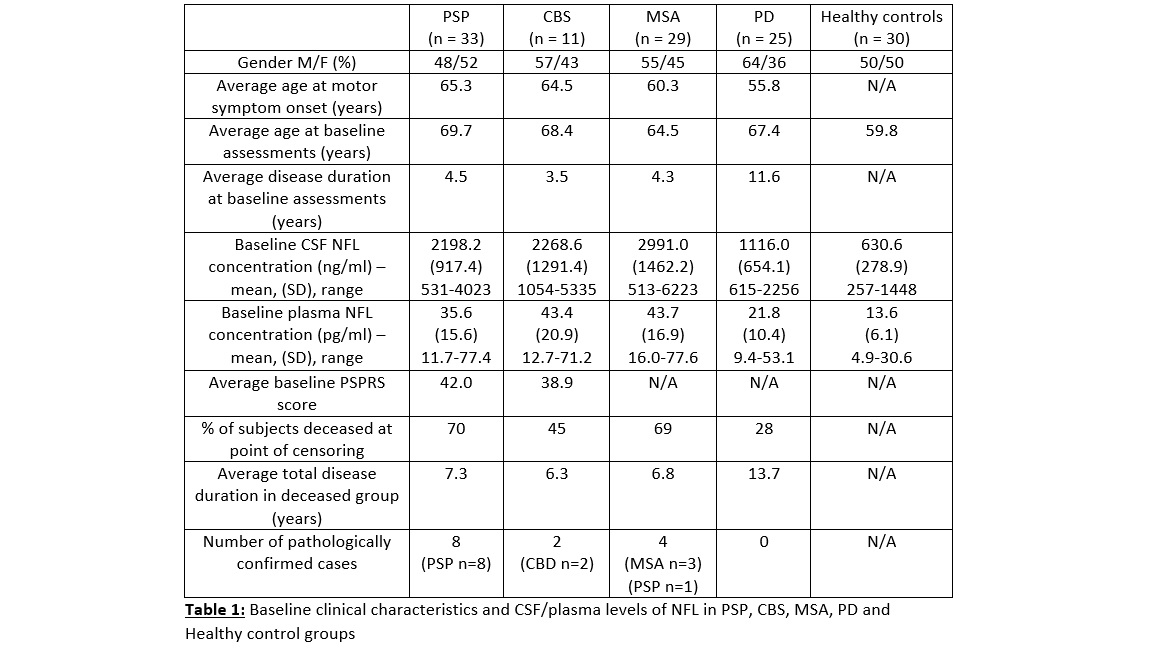
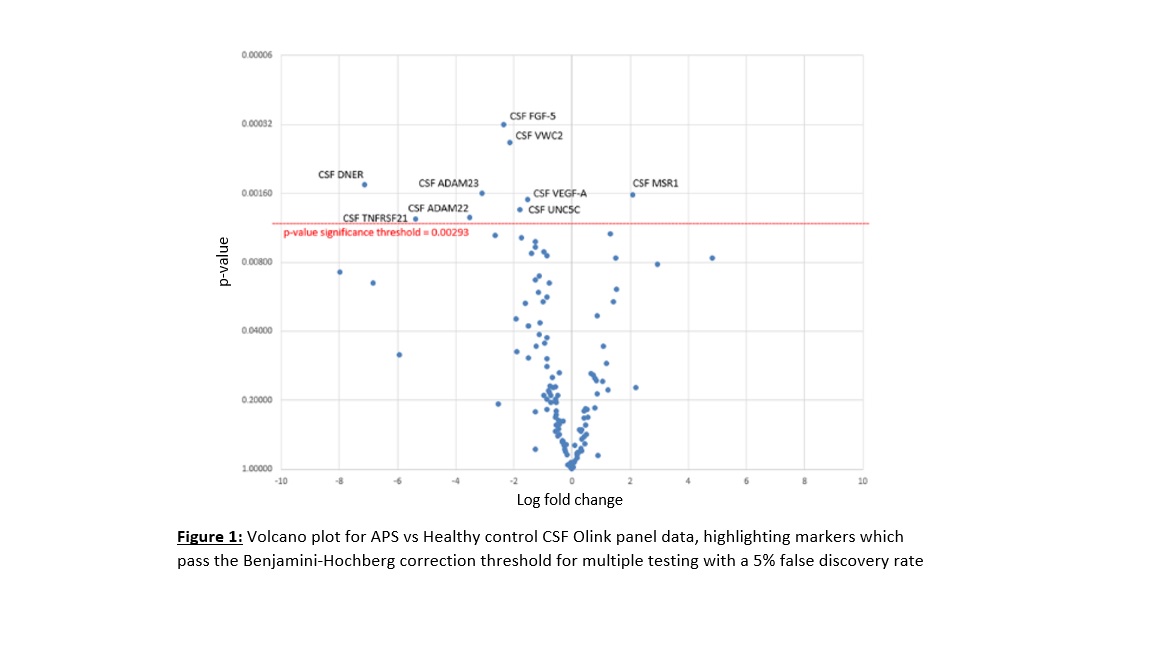
Methods: A cohort of patients and healthy controls were recruited at the National Hospital for Neurology and Neurosurgery, London, and followed up longitudinally. Patients were assigned diagnoses according to current clinical diagnostic criteria. Clinical progression data was extracted from clinical notes at the point of censoring. A subset of deceased patients underwent neuropathological diagnosis at the Queen Square Brain Bank, London. Baseline CSF and plasma samples underwent single molecule array testing for NFL levels and Olink Neurology and Inflammation panel testing using multiplex proximity extension assay technology. PSP, CBS and MSA subjects were combined to form one “APS” group. APS vs control group comparisons for Olink panel data were performed using logistic regression analyses that used gender and age at the point of testing as covariates.
Results: Baseline clinical characteristics and CSF/plasma NFL levels in our cohort is summarised below (Table 1). None of the Olink panel plasma markers passed the significance threshold for differentiating APS from controls. The results for Olink panel CSF markers are shown in the volcano plot below (Figure 1). Every significant CSF marker, with the exception of MSR1, was also significant in differentiating APS from PD using similar logistic regression models. Levels of FGF-5, ADAM 22+23, DNER and VEGF-A showed linear relationships (p<0.05) with levels of both CSF and plasma NFL.
Conclusions: Our most promising markers were all downregulated in APS compared to both PD and controls and the biological processes regulated by them include cell differentiation/apoptosis, immune cell migration and neural development. We plan on replicating our findings using clinical and biomarker data from our PROSPECT-M-UK study. This is the largest ever longitudinal study that tracks the clinical progression of APS patients over 5 years.
References: (1) Hall S, Öhrfelt A, Constantinescu R, et al. Accuracy of a panel of 5 cerebrospinal fluid biomarkers in the differential diagnosis of patients with dementia and/or Parkinsonian disorders. Arch Neurol 69, 1445 (2012). (2) Rojas JC, Karydas A, Bang J, et al. Plasma neurofilament light chain predicts progression in progressive supranuclear palsy. Ann Clin Transl Neurol 3, 216-225 (2016).
To cite this abstract in AMA style:
E. Jabbari, J. Woodside, N. Magdalinou, A. Lees, H. Zetterberg, H.. A panel of CSF and plasma biomarkers reveals novel biological insights into atypical parkinsonian syndromes [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/a-panel-of-csf-and-plasma-biomarkers-reveals-novel-biological-insights-into-atypical-parkinsonian-syndromes/. Accessed January 17, 2026.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/a-panel-of-csf-and-plasma-biomarkers-reveals-novel-biological-insights-into-atypical-parkinsonian-syndromes/