Session Information
Date: Sunday, October 7, 2018
Session Title: Parkinsonism, MSA, PSP (Secondary and Parkinsonism-Plus)
Session Time: 1:45pm-3:15pm
Location: Hall 3FG
Objective: To introduce a very old woman case of Sjögren´s syndrome (SS) and Parkinsonism as well as to review previously reported cases.
Background: Movement disorders have been associated with a variety of autoimune diseases. SS is a common autoimune disorder, characterized by lymphocytic infiltration and destruction of the salivar and lachrymal glands leading to dry eyes and dry mouth (sicca syndrome) with positive anti-Ro/SSA and anti-La/SSB antibodies. The nervous system may be involved in approximately 31% of patients with SS. The mechanism of neurologic damage is thought to be secondary to a vasculopathy or antineuronal antibodies. Findings suggestive of vasculopaty in Magnetic Resonance Imaging (MRI) studies may be present or not. Treatment can be attempted with corticosteroids or L-dopa with variable response. Few studies have described such association and there are still many unanswered questions about it.
Methods: Case report and a systematic review of the literature was performed. The MEDLINE database, available through PubMed web-site, has been queried using “Parkinsonism” and “Sjögren´s syndrome” as key words. The search was limited considering only papers describing an association between the two diseases in English language.
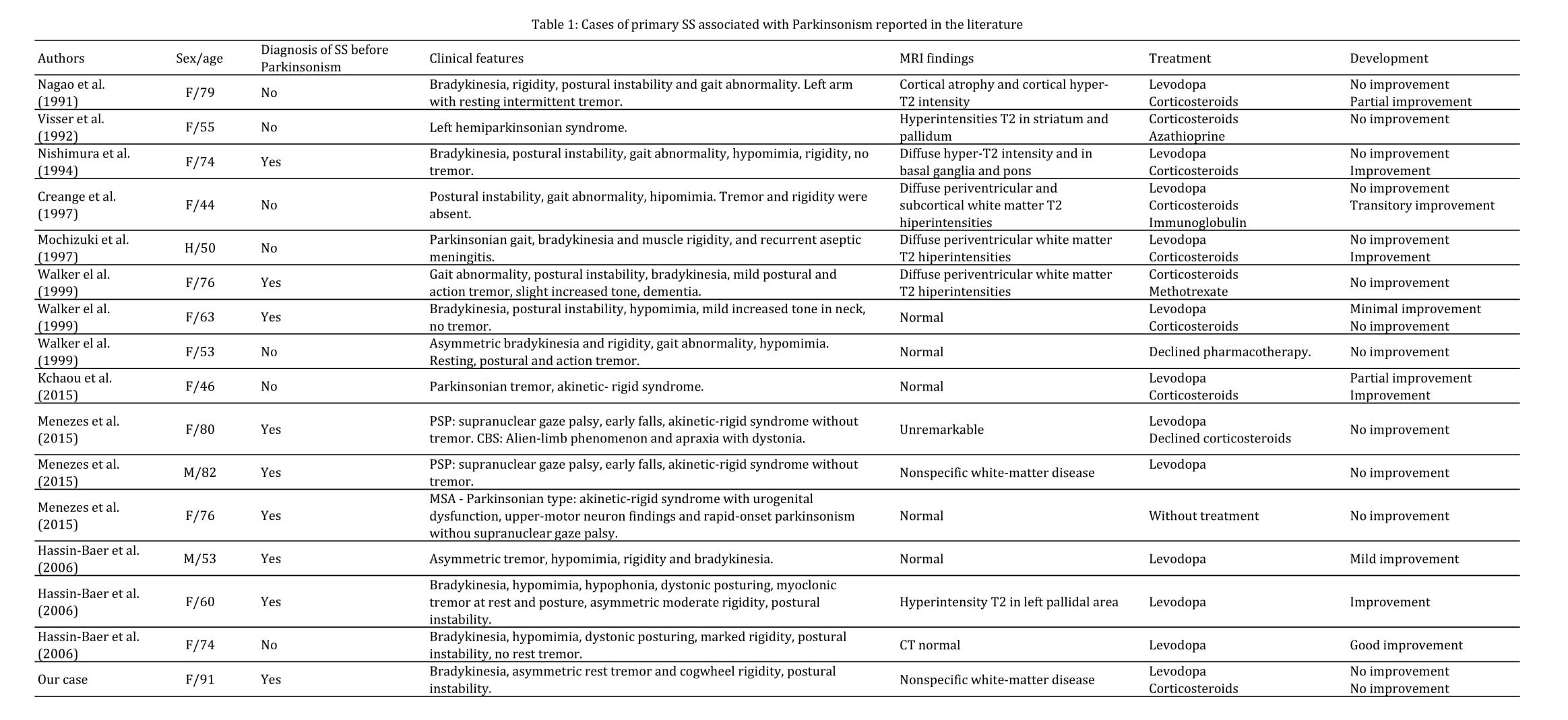
Results: 91 years old female patient, first evaluation for allergic lesions on her skin and leukopenia. Sicca syndrome and Raynaud´s phenomenon were present. Exams revealed anti-Ro/SSA in high titers and anti-La/SSB and antinuclear antibodies (1:640) positive. Six moths later she developed a rapid onset of parkinsonism: bradykinesia, postural instability, asymmetric cogwheel rigidity and rest tremor. There were not supranuclear gaze palsy, dysautonomia, apraxia or dystonia. She was referred to a neurologist. Brain MRI revealed nonspecific white matter alterations and slightly high protein in CSF. We prescribed prednisone and levodopa with no improvement. After 2 years of follow up she developed dysphagia, dementia and imobility. We found 15 cases reported in the literature (table1) and one nationwide case-control study from Taiwan. The last one classified patients with Parkinson´s disease and did not describe these clinical features.
Conclusions: Few studies have described associaton of SS and parkinsonism. To the best of our knowledge, this one reports the oldest patient. Clinical features and MRI findings are variable, as well as treatment response. Further longitudinal studies are necessary to improve knowledge about this association and establish the best therapies.
References: Menezes, R., Pantelyat, A., Izbudak, I., & Birnbaum, J. (2015). Movement and Other Neurodegenerative Syndromes in Patients with Systemic Rheumatic Diseases: A Case Series of 8 Patients and Review of the Literature. Medicine, 94(31). Kchaou, M., Ben Ali, N., Hmida, I., Fray, S., Jamoussi, H., Jalleli, M., … & Belal, S. (2015). Parkinsonism and Sjögren’s Syndrome: A Fortuitous Association or a Shared Immunopathogenesis?. Case reports in medicine, 2015.
To cite this abstract in AMA style:
M. Augusto, PV. Perin. 91 years old woman with Sjogren’s syndrome and Parkinsonism [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/91-years-old-woman-with-sjogrens-syndrome-and-parkinsonism/. Accessed April 1, 2025.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/91-years-old-woman-with-sjogrens-syndrome-and-parkinsonism/