Session Information
Date: Saturday, October 6, 2018
Session Title: Surgical Therapy: Parkinson's Disease
Session Time: 1:45pm-3:15pm
Location: Hall 3FG
Objective: To analyzse the effect of low frequency (LFS) subthalamic nucleus deep brain stimulation (STN-DBS) on speech and voice in Parkinson’s disease (PD) patients with medium/long term post-surgical follow-up.
Background: STN-DBS has an optimal effect on cardinal motor symptoms of PD. Nevertheless, its long-term effect on dysarthria is not clear. Few studies, with small patients samples, suggest a transient beneficial effect of LFS on PD dysarthria. Though data in this area are scarce [1].
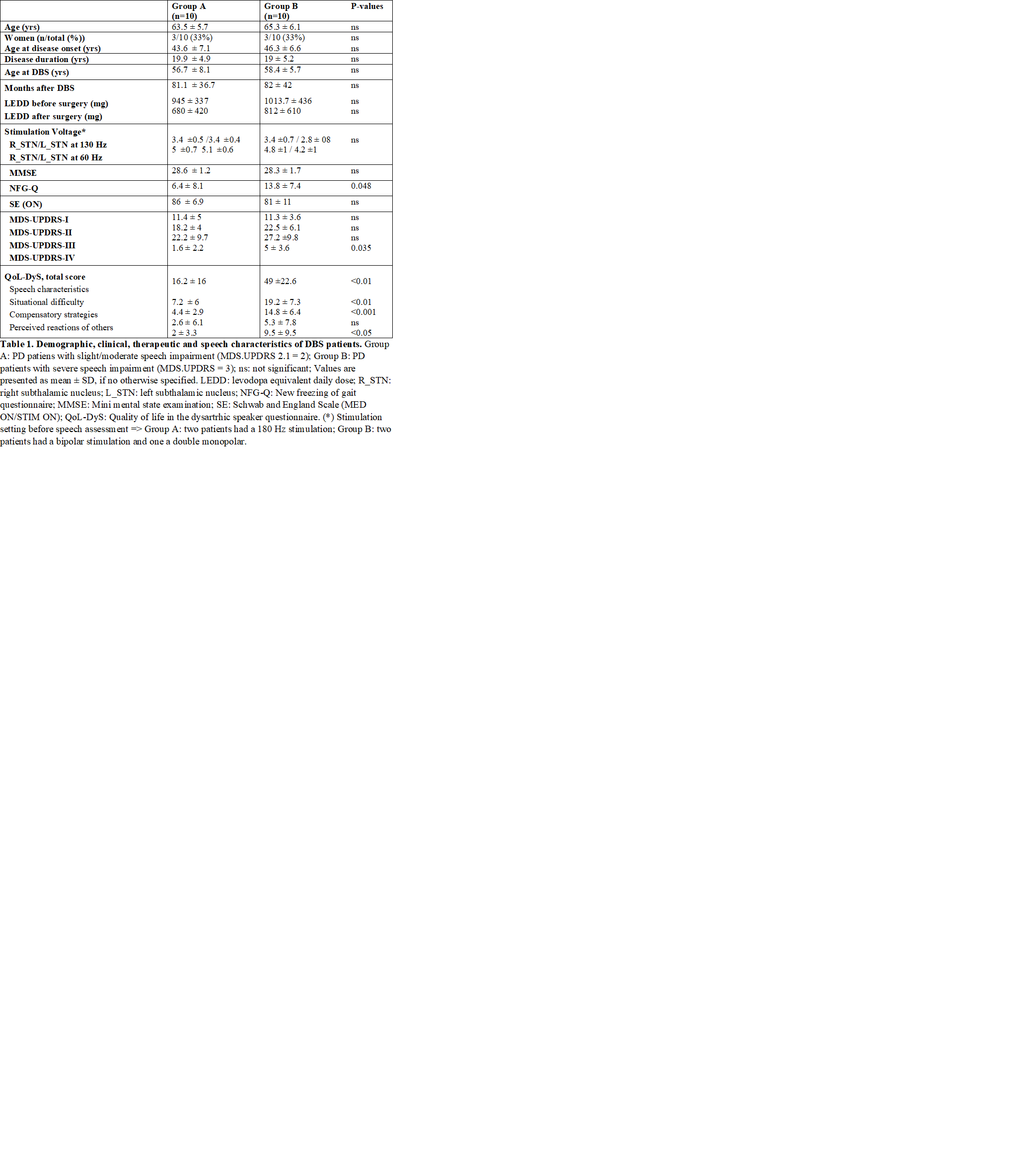
Methods: 20 PD patients who underwent STN-DBS at least 3 years before, divided into two groups, matched for gender, age and age at disease onset (Group A: slight speech impairment [MDS-UPDRS item 2.1 ≤ 2] and group B: severe speech impairment [MDS-UPDRS item 2.3 ≥ 3] were tested in the following conditions: MED OFF/STIM ON (130Hz – standard frequency), MED OFF/STIM OFF and MED OFF/STIM ON (60Hz – LFS). Total electrical energy delivered was maintained constant. The following was assessed in all conditions: maximum phonation time, voice quality and stability, oral diadochokinesis, speech rate and intelligibility and MDS-UPDRS-III. Voice samples were recorded and analyzed by a speech pathologist, blinded to patients’ therapeutic condition. A two weeks follow-up was performed in patients who decide to keep LFS due to a subjective and clinician rated acute improvement of speech and voice.
Results: Overall, mean (SD) age was 64.4 (±5.8) years and mean disease duration 19.4 (±4.5) years. Data on demographic, clinical, therapeutic characteristics and speech impairment impact on quality of life, are detailed in Table 1 [Table 1]. LFS compared to no stimulation (MED OFF/STIM ON at 60Hz vs MED OFF/STIM OFF) significantly improved voice quality, diadococinesis and intelligibility in Group A and diadococinesis and intelligibility in Group B, with a motor improvement (MDS-UPDRS-III) of 42±12% and 39± 22% in the two groups, respectively. On the other hand, when comparing LFS to standard frequency stimulation, there was a significant improvement of maximum phonation time, diadococinesis and intelligibility only in Group B without significant changes of motor performance. Five Group B patients opted to maintain LFS. At two weeks follow-up, two of them were kept at 60Hz stimulation, one was switched to 80 Hz and two were switched back to 130Hz, due to tremor and wearing-off reappearance.
Conclusions: LFS could be a useful option to test for STN-DBS patients with severe speech impairment. Nevertheless, its effect on motor symptoms and motor fluctuations may not be preserved over time.
References: [1] Moreau C, Pennel-Ployart O, Pinto S, Plachez A, Annic A, Viallet F, Destée A, Defebvre L. Modulation of dysarthropneumophonia by low-frequency STN DBS in advanced Parkinson’s disease. Mov Disord. 2011 Mar;26(4):659-63.
To cite this abstract in AMA style:
M. Fabbri, M. Zibetti, G. Ferrero, A. Accornero, I. Guimaraes, M. Rizzone, A. Romagnolo, J. Ferreira, L. Lopiano. Is lowering stimulation frequency a feasible option to improve speech in Parkinson’s disease patients undergoing subthalamic deep brain stimulation? [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/is-lowering-stimulation-frequency-a-feasible-option-to-improve-speech-in-parkinsons-disease-patients-undergoing-subthalamic-deep-brain-stimulation/. Accessed April 1, 2025.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/is-lowering-stimulation-frequency-a-feasible-option-to-improve-speech-in-parkinsons-disease-patients-undergoing-subthalamic-deep-brain-stimulation/