Session Information
Date: Saturday, October 6, 2018
Session Title: Parkinson’s Disease: Clinical Trials, Pharmacology And Treatment
Session Time: 1:45pm-3:15pm
Location: Hall 3FG
Objective: To evaluate if a multi-disciplinary PD clinic can result in better outcome in PD patients in 2 years.
Background: PD is a neurodegenerative disease affecting both motor and non-motor domains. Therefore, a multi-disciplinary management model, which can address both symptoms, should be a preferable management model in chronic neurodegenerative diseases like PD. However, evidence studying this area is scarce.
Methods: Study design: Prospective observational study conducted in the multidisciplinary PD clinic of Queen Elizabeth Hospital of Hong Kong between October 2014 and January 2018. Inclusion criteria: 1. A clinical diagnosis of PD based on the UK Brain Bank criteria. 2. Ability to complete the study questionnaires. 3. Written informed consent signed. Method: 1. The subjects were evaluated at baseline and 2 years after joining the out-patient multidisciplinary care program. 2. The demographic information was documented. 3. Functional status and quality of life (QoL) are the primary outcomes whereas motor and non-motor functions serve as the secondary outcomes. 4. SPSS version 20 was used for statistical analysis. 5. Chi square and t tests were used to test for differences.
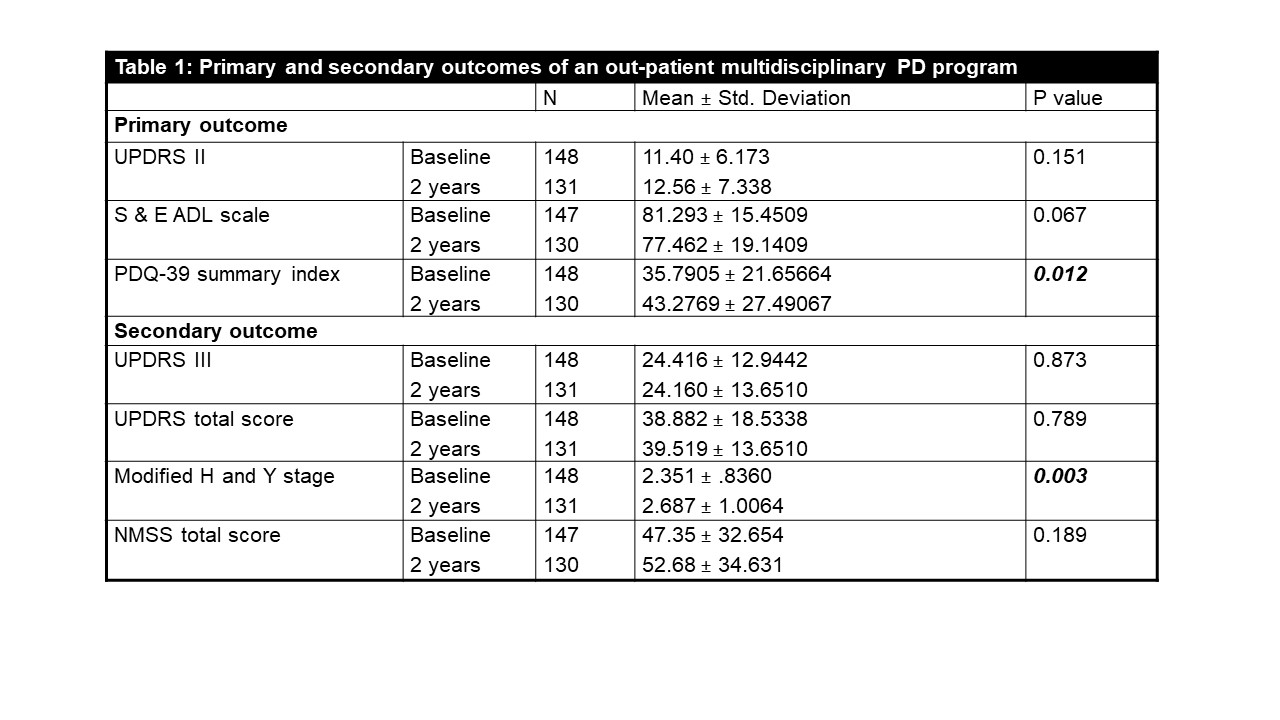
Results: 152 subjects were recruited. – 5 subjects were excluded because of wrong diagnosis / patient’s refusal / severe dementia. – There were 17 dropouts because of patient’s refusal and death. – Primary outcome: There was no significant difference in the functional status (in terms of Unified Parkinson’s Disease Rating Scale (UPDRS) part II and Schwab and England Activities of Daily Living Scale (S&E ADL scale)) in the subjects at baseline and 2 years after enrollment. However, as compared with the QoL (as measured by the 39-item Parkinson’s Disease Questionnaire (PDQ-39) summary index) at baseline, it was found to be worse 2 years after joining the program (Table 1). Secondary outcome: There was no significant difference in the motor (in terms of UPDRS part III and modified Hoehn and Yahr (H&Y) stage) and non-motor (in terms of Non-Motor Symptoms Scale (NMSS)) function of the participants at baseline and 2 years after joining the program (Table 1).
Conclusions: This study reported that this multi-disciplinary clinic could not improve the functional status and QoL of PD patients. Further research using control groups may be useful to evaluate if multi-disciplinary management can delay disease progression in PD.
To cite this abstract in AMA style:
G. Chan, N. Cheung, S. Or, I. Chan, A. Leung, C. Li, D. Chau, C.W. Woo, B. Chee, W.C. Fong. Effectiveness of a Multi-disciplinary Parkinson’s Disease (PD) Clinic: A 2-year Prospective Observational Study [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/effectiveness-of-a-multi-disciplinary-parkinsons-disease-pd-clinic-a-2-year-prospective-observational-study/. Accessed April 1, 2025.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/effectiveness-of-a-multi-disciplinary-parkinsons-disease-pd-clinic-a-2-year-prospective-observational-study/