Session Information
Date: Wednesday, June 22, 2016
Session Title: Parkinson's disease: Neuroimaging and neurophysiology
Session Time: 12:00pm-1:30pm
Location: Exhibit Hall located in Hall B, Level 2
Objective: To determine structural connectivity between the mesencephalic locomotor region (MLR) and the supplementary motor area (SMA) in freezers compared to non-freezers.
Background: Freezing of Gait (FoG) is a debilitating, progressive and common phenomenon occurring in Parkinson’s disease (PD) patients. The pathophysiology of FoG is poorly understood, and there are no effective therapies. Loss of automaticity of gait via degeneration of MLR is a proposed hypothesis. We further hypothesize that cortical control of gait occurs as a compensatory response to this loss of automaticity. The SMA cortical region has extensive basal ganglia connections and has been implicated in self-initiated movements as well as executive functions, which have been strongly associated with FoG.
Methods: 19 PD patients without FoG and 16 PD with FoG underwent MRI studies with diffusional kurtosis imaging (DKI). A deterministic fiber-tracking algorithm based on DKI was used, with a seeding region placed at the pedunculopontine nucleus (PPN) to the ending region at the SMA, see figure 1. The anisotropy threshold for all subjects ranged from 0.08 to 0.10, angular threshold at 60 degrees, and step size at 1.5 mm. Tracks with length less than 60 mm were discarded and a total of 10000 seeds were placed. 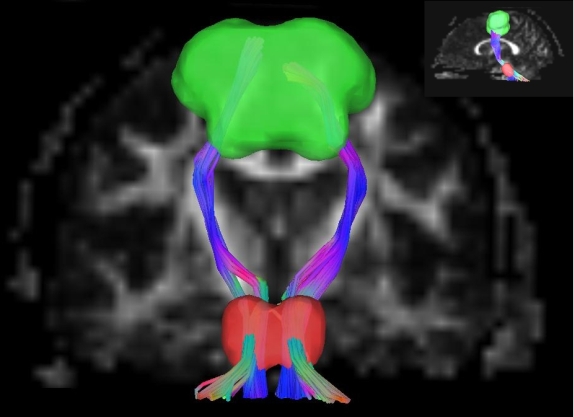
Results: PD non-freezers had mean age of 70 years and were 79% male, while PD freezers had a mean age of 65.7 years and were 69% male. Freezers had increased fiber count (mean=1599.69 SD 685.48) compared to non-freezers (mean=1073 SD 628), p=0.025, see figure 2. Tract volume, tract length, and quantitative anisotropy were not significantly different between groups. There was no significant difference between dopa-responsive and dopa-unresponsive freezers. 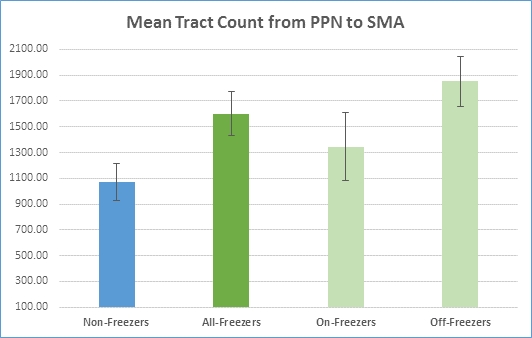
Conclusions: This data supports the notion that there is increased cortical control of gait in patients with PD and FoG compared to non-freezers. Further studies to determine whether or not this change is compensatory or maladaptive are warranted.
To cite this abstract in AMA style:
G.J. Revuelta, C. Chan, S. Jenkins, J. Jensen, L. Bonilha. Increased cortical control of gait in patients with Parkinson’s disease and freezing of gait [abstract]. Mov Disord. 2016; 31 (suppl 2). https://www.mdsabstracts.org/abstract/increased-cortical-control-of-gait-in-patients-with-parkinsons-disease-and-freezing-of-gait/. Accessed February 2, 2026.« Back to 2016 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/increased-cortical-control-of-gait-in-patients-with-parkinsons-disease-and-freezing-of-gait/
