Session Information
Date: Thursday, June 8, 2017
Session Title: Parkinson's Disease: Neuroimaging And Neurophysiology
Session Time: 1:15pm-2:45pm
Location: Exhibit Hall C
Objective: To determine white matter abnormalities in PD patients with various degrees of olfactory impairment.
Background: Neuroimaging results of PD brain based on diffusion tensor imaging(DTI)correlate well with the olfactory loss in PD patients.In the present study we aim to determine whether white matter integrity measured based on DTI method is associated with odor identification test scores in PD patients.
Methods: Data used in the preparation of this article were obtained from the Parkinson’s Progression Markers Initiative (PPMI) database. Odor identification was assessed using the University of Pennsylvania Smell Identification Test(UPSIT).
Five groups, total 85 subjects (18 anosmia, 26, 17 and 12 PD patients with severe, moderate and mild microsmia, respectively and 12 PD patients with normal olfactory status) were recruited with similar age, sex ratio, GDS, MoCA, handed and NHY.
The Diffusion MRI data were corrected for subject motion, eddy current distortions, and susceptibility artefacts due to the magnetic field inhomogeneity using Explore DTI toolbox [2]. Diffusion MRI connectometry was conducted in all subgroups using a multiple regression model considering UPSIT, sex, age and the local significant connectomes.
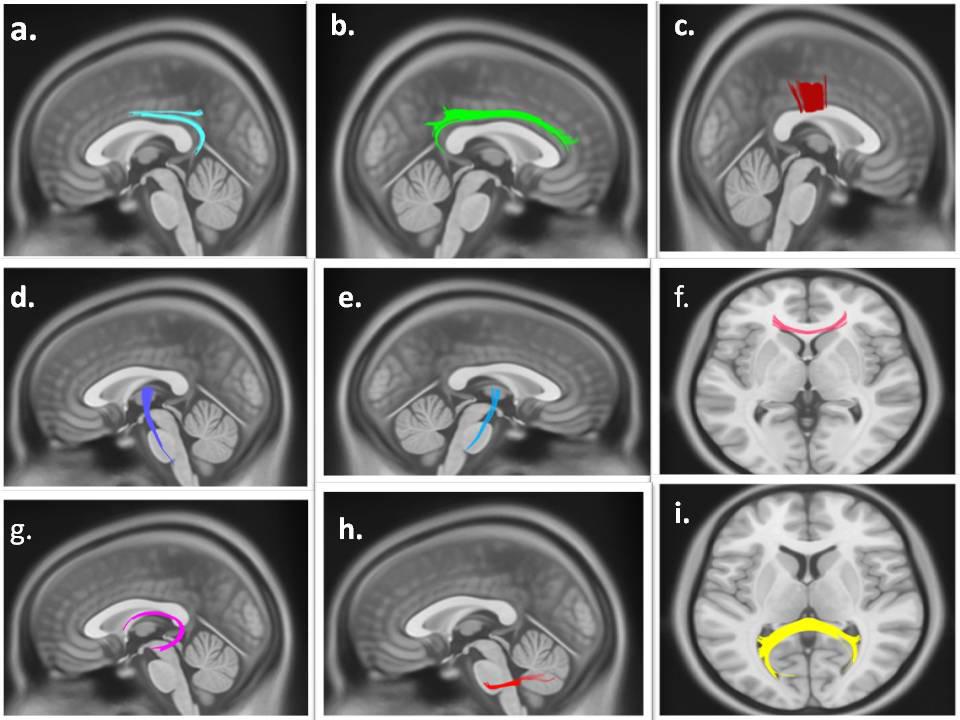
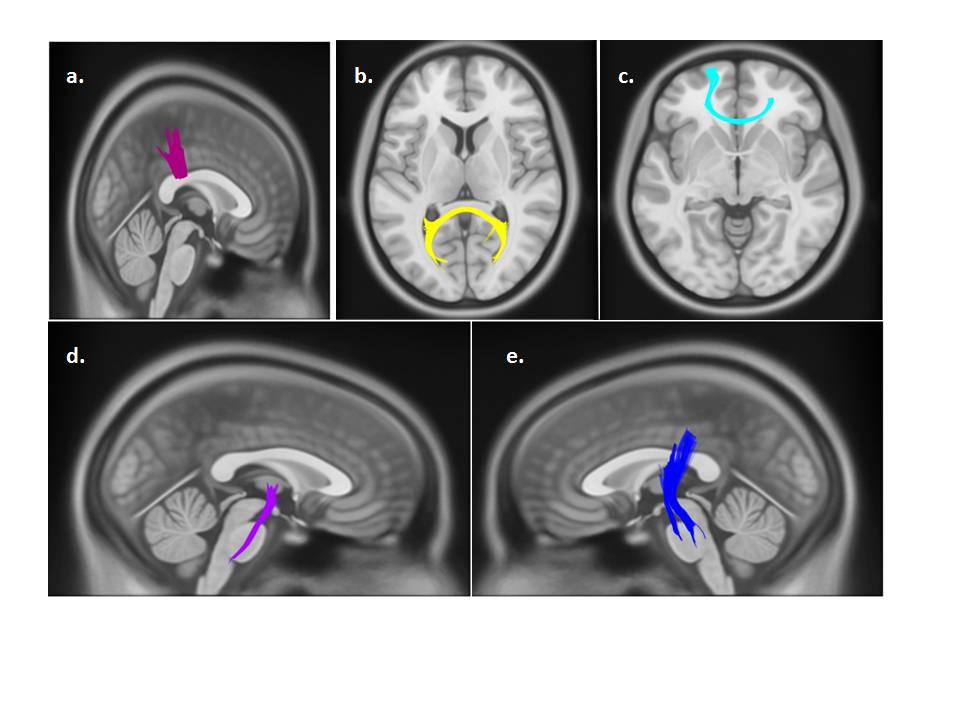
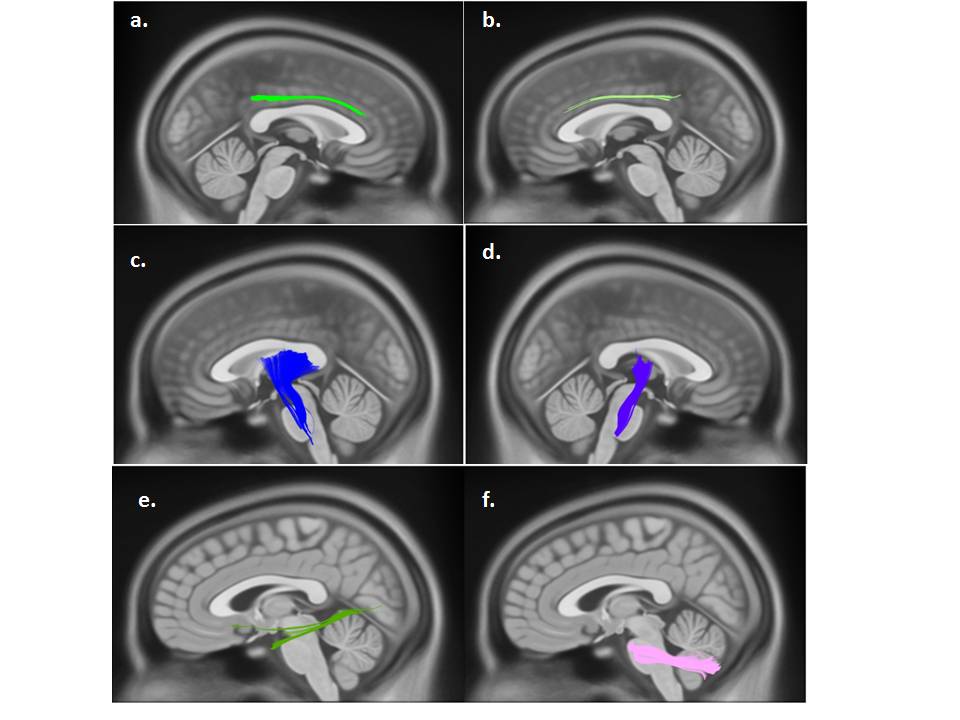
Results: The between-group Connectometry revealed that individuals with PD-Anosmia had lower QA(FDR=0.02123)in body of the corpus callosum (CC),bilateral corticospinal tracts,middle cerebellar peduncles,right and left cingulate cortex,left fornix,Genu and splenium of corpus callosum compared to patients with mild microsmia[Figure 1].A significant difference(FDR=0.04683)was observed in body,Genu and Splenium of the corpus callosum(CC)and bilateral corticospinal tracts between PD-anosmia and patients with moderate microsmia[Figure 2].individuals with Severe microsmia had alterations in FA in multiple regions(FDR=0.07658),including the right and left cingulate cortex, bilateral corticospinal tracts, middle cerebellar peduncles and left inferior longitudinal fasciculus(ILF)compared to mild microsmia patients[Figure 3].
Conclusions: This study shed light on the microstructural changes in bilateral cingulum, CC, IFOF, CST and MCP areas associated with olfactory impairment in early diagnosed PD patients. Since smell insufficiency is the precursor to PD, microstructural changes regarding reduced FA values in olfactory regions might reflect the primitive alterations in Parkinsonic brain.
References: 1. Ibarretxe-Bilbao, N., et al., Olfactory impairment in Parkinson’s disease and white matter abnormalities in central olfactory areas: A voxel-based diffusion tensor imaging study. Mov Disord, 2010. 25(12): p. 1888-94.
2. Doty, R.L., et al., University of Pennsylvania Smell Identification Test: a rapid quantitative olfactory function test for the clinic. Laryngoscope, 1984. 94(2 Pt 1): p. 176-8.
To cite this abstract in AMA style:
S. Sobhani, M. Aarabi. Olfactory Impairment in Parkinson’s Disease and White Matter Abnormalities in Central Olfactory Areas [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/olfactory-impairment-in-parkinsons-disease-and-white-matter-abnormalities-in-central-olfactory-areas/. Accessed December 27, 2025.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/olfactory-impairment-in-parkinsons-disease-and-white-matter-abnormalities-in-central-olfactory-areas/