Session Information
Date: Wednesday, June 7, 2017
Session Title: Phenomenology and Clinical Assessment Of Movement Disorders
Session Time: 1:15pm-2:45pm
Location: Exhibit Hall C
Objective: To examine a case of comorbid normal pressure hydrocephalus (NPH) with Parkinson’s Disease (PD).
Background: PD and NPH are the most common high level gait disorders in the elderly. The pathophysiology of parkinsonian symptoms in NPH has not been identified. Odagiri retrospectively analyzed the findings on iodine-123-meta-iodobenzylguanidine SPECT in 21 patients with definite diagnosis of NPH. One third showed signs of sympathetic cardiac denervation, indicating a potentially associated alpha-synucleinopathy [1]. Importantly, NPH is a treatable neurological disorder.
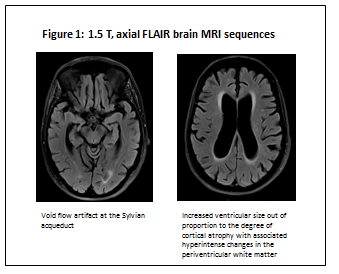
Methods: A 79 year-old woman presented with a 2 years history of mild left-hand tremor, asymmetric bradykinesia, rigidity and mild freezing of gait (FoG). Her UPDRS Motor Score was 34. Carbidopa/Levodopa was initiated without subjective benefits despite objective improvement of appendicular bradykinesia. In the following months she showed a significant gait impairment with unsteadiness, frequent falls, severe FoG out of proportion to her mild parkinsonism. She also reported occasional urge incontinence. Neuropsychiatric evaluation showed moderate executive impairment. A brain MRI showed ventriculomegaly disproportionate to sulcal enlargement, callosal angle of 63°, flow-void at the aqueduct and confluent T2-hyperintense changes in the periventricular white matter (fig.1).
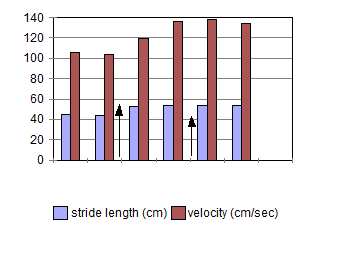
Results: A large volume tap provided a significant improvement in gait and balance, leading to a ventricular-peritoneal shunt. Video gait analysis was performed on a distance of 60 feet with post-processing of gait parameters; six months post-shunt assessment showed significant improvement in all parameters (fig. 2). The UPDRS-II FoG item improved from 2 to 0, UPDRS-III from 34 to 13. Montreal Cognitive Assessment improved by 3 points. FoG, falls and urinary disturbances resolved. She has persistent, mild, asymmetric bradykinesia and rigidity.
Conclusions: We report a case of levodopa-responsive parkinsonism with overlapping NPH. While appendicular bradykinesia mildly improved with dopaminergic therapy, axial symptoms and locomotion dramatically responded to shunt placement. The time lapse between clinical onset and shunting is a critical prognostic factor. Clinicians should be aware of the potential coexistence of these two pathologies to promptly provide the most effective treatment.
References: Odagiri H, Baba T, Nishio Y, Iizuka O, Narita W, Matsuda M, Mori E. Clinical characteristics of idiopathic normal pressure hydrocephalus with Lewy body diseases. J Neurol Sci. 2015 Dec 15;359(1-2):309-11
To cite this abstract in AMA style:
A. Cucca, M. Biagioni, J. Golomb, J. Fleisher. Comorbid Normal Pressure Hydrocephalus with Parkinson’s disease: a call for clinical awareness [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/comorbid-normal-pressure-hydrocephalus-with-parkinsons-disease-a-call-for-clinical-awareness/. Accessed January 4, 2026.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/comorbid-normal-pressure-hydrocephalus-with-parkinsons-disease-a-call-for-clinical-awareness/