Session Information
Date: Wednesday, June 7, 2017
Session Title: Ataxia
Session Time: 1:15pm-2:45pm
Location: Exhibit Hall C
Objective: To report a 26 year-old female with progressive cerebellar ataxia for 12 years diagnosed to have primary progressive multiple sclerosis (PPMS).
Background: Multiple sclerosis (MS) is a kind of CNS demyelinating disease. About 15% MS patients have a progressive course without a relapsing course. These patients are considered to have PPMS. It often presented a progressive neurological problem–such as lateralizing weakness, or numbness in the legs. Cerebellar ataxia as primary symptom is less frequent in PPMS and it’s usually diagnosed in their 40-60 years at age. Here we present a case with adolescent-onset PPMS presenting progressive cerebellar ataxic syndrome.
Methods: A 26 year-old female Taiwanese presented with 12 years of progressive ataxic gait. She denied relapses and remissions of symptoms. There were no mental decline, involuntary movements, muscle hypertrophy or abnormality in hearing or vision. She had no associated family history or consanguineous parents. Physical examination revealed dysarthria, dysmetria/intentional tremor and dysdiadochokinesia in four limbs and bilateral extensor plantar response. In addition, she had normal tendon reflexes, intact sensory function and negative Romberg test without parkinsonian features. Her gait was wide-based.
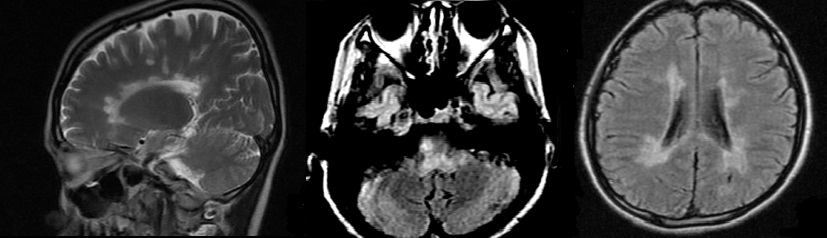
Results: On investigation, CBC, lipid profile, LFT, chest X-ray, serum electrolytes, ECG, EEG and NCV showed normal results. VEP study were abnormal. The brain and cervical spine MRI showed no significant cerebellar atrophy or myelopathy. Instead, FLAIR-weighted imaging showed diffuse plaques in brainstem and cerebral white matters with a predilection for periventricular white matter with the major axes perpendicular to the ventricular surface (Dawson’s fingers). Besides, the CSF study revealed oligoclonal banding and elevation of IgG index. She had normal serum copper and ceruloplasmin levels and plasma very long-chain fatty acids (VLCFA) analysis. The genetic testing for spinocerebellar ataxia ( SCA1, 2, 3, 6, 7 and 17) is negative. In view of progressive ataxia with diffuse white matter lesions, a diagnosis of PPMS was made.
Conclusions: PPMS can be a etiology in adolescent patient with progressive ataxic syndrome. Brain MRI is a better tool for detecting cerebral white matter lesions compared to CT in differential diagnosis of progressive ataxia.
References:
- AJNR June 2006 27: 1165-1176
- Lancet Neurol 2007; 6: 903–12
To cite this abstract in AMA style:
S.-K. Yang, J.-J. Lin. A case report: a primary progressive multiple sclerosis (PPMS) with adolescent-onset of progressive cerebellar ataxia [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/a-case-report-a-primary-progressive-multiple-sclerosis-ppms-with-adolescent-onset-of-progressive-cerebellar-ataxia/. Accessed March 29, 2025.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/a-case-report-a-primary-progressive-multiple-sclerosis-ppms-with-adolescent-onset-of-progressive-cerebellar-ataxia/