Session Information
Date: Wednesday, June 22, 2016
Session Title: Neuroimaging (non-PD)
Session Time: 12:00pm-1:30pm
Location: Exhibit Hall located in Hall B, Level 2
Objective: To evaluate in vivo signs of gray matter (GM) and white matter (WM) abnormalities, through an unbiased neuroimaging method, in a large cohort of patients with SPG11, and correlate these findings with physical disability.
Background: Hereditary Spastic Paraplegia constitutes a group of rare monogenic disorders, characterized by progressive spasticity and paraparesis. SPG11 is the main cause of autosomal recessive HSP. Thinning of the corpus callosum and the “Ears of Lynx” sign are key neuroimaging features. Clinically, the majority of patients demonstrate cognitive deficits, together with pleomorphic neurological abnormalities such as movement disorders and psychiatric symptoms. These features suggest a more widespread neuronal damage than what can be accessed through conventional MRI.
Methods: Nineteen patients with confirmed SPG11 from 11 different kindreds (mean age: 29.1±8.3 years, 9 men) were recruited from the neurology outpatient clinic of University of Campinas and Federal University of São Paulo, Brazil. Motor impairment was quantified through the Spastic Paraplegia Rating Scale (SPRS). Imaging findings were compared with 19 age and sex-matched controls. All subjects underwent 3T MRI scans. T1 volumetric sequences (1mm) were analyzed through voxel based morphometry (VBM). Processed images were compared between patients and controls to identify areas of WM and GM volumetric loss. Voxelwise statistical analyses were performed and significant differences were set at α≤0.001 corrected for multiple comparisons using a false discovery rate of 5%.
Results: All patients presented with progressive spastic paraplegia, 15 were already wheelchair bound and 16 had significant cognitive impairment. Mean age of onset was 16.3+-2.9 and mean disease duration was 12.8+-8. Mean SPRS was 31.6+-11.9. VBM analysis identified symmetrical and diffuse WM volumetric reduction affecting all supra and infratentorial WM regions 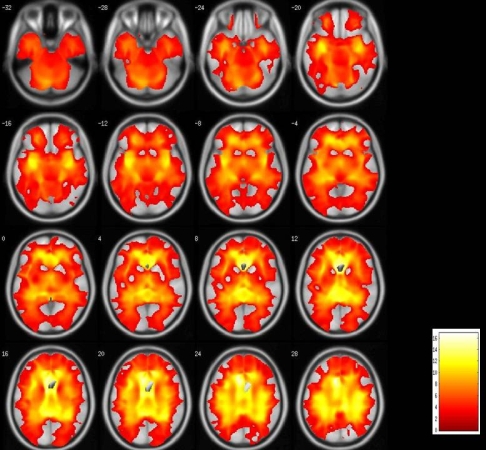 . GM volumetric reduction in patients affected all deep gray matter structures. Cortical areas predominantly affected were frontal and temporal lobes, together with the cyngulate gyrus
. GM volumetric reduction in patients affected all deep gray matter structures. Cortical areas predominantly affected were frontal and temporal lobes, together with the cyngulate gyrus 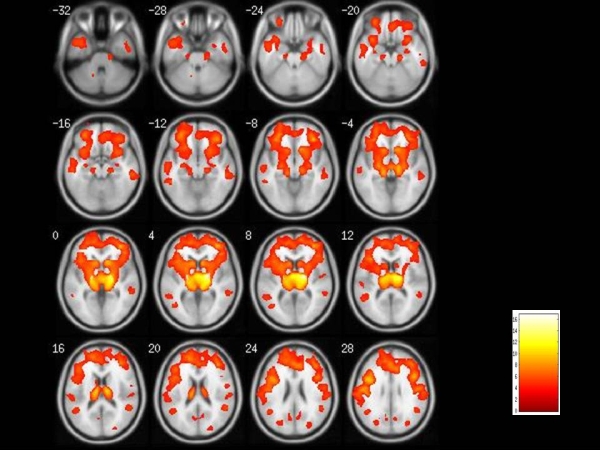 . Frontal lobe WM reduction correlated with greater SPRS scale.
. Frontal lobe WM reduction correlated with greater SPRS scale.
Conclusions: Widespread WM and deep GM volume loss was observed in SPG11 patients. Frontal WM damage correlates with motor disability and might be a potential neuroimaging marker to assess disease progression.
To cite this abstract in AMA style:
I. Faber, A.R.M. Martinez, T.T.J. Rezende, R.F. Casseb, C.M. Lourenço, W. Marques Jr, J.L. Pedroso, O.G.P. Barsottini, I.T. Lopes-Cendes, M.C. França Jr. Frontal lobe white matter atrophy correlates with disability in spastic paraplegia type 11 (SPG11) [abstract]. Mov Disord. 2016; 31 (suppl 2). https://www.mdsabstracts.org/abstract/frontal-lobe-white-matter-atrophy-correlates-with-disability-in-spastic-paraplegia-type-11-spg11/. Accessed April 3, 2025.« Back to 2016 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/frontal-lobe-white-matter-atrophy-correlates-with-disability-in-spastic-paraplegia-type-11-spg11/
