Session Information
Date: Monday, June 5, 2017
Session Title: Parkinsonism, MSA, PSP (Secondary and Parkinsonism-Plus)
Session Time: 1:45pm-3:15pm
Location: Exhibit Hall C
Objective: Differentially diagnosing subgroups in Parkinsonism for optimal rehabilitation thus designed study with real-time dynamic magnetic resonance imaging (MRI) and automated acoustic analysis
Background: In Parkinsonism with progressive degeneration skilled articulatory and respiratory motor programs deteriorate leading to axial features. Agonist-antagonist muscle groups lead to perceptual features hypothesized to be significantly different in Parkinson’s Disorder (PD), multiple system atrophy (MSA) and progressive supranuclear palsy (PSP). Promising instrument for differential diagnosis may be MRI (spatio-temporal articulatory dynamics)[1] and automated acoustic features analysis with support vector machines (SVM)[2]
Methods: Investigations involved clinical assessments (UPDRS-III, H&Y, UMSARS, PSPRS, PDQ39); dynamic MRI to visualize vocal tract during speech production and automated analysis of audio-recorded speech. Compared natural rate Hindi syllable production (unaspirated, voiceless/voiced) in healthy control, PD, MSA and PSP (age 45-70 years) with 2-D single slice MRI using ‘trufi’ sequence (acquisition time of 80s) at 1.5T MR scanner (Avanto, Siemens, Germany) with 12-channel head & neck coil using SuperLab4.2, Cedrus Inc.USA and MR compatible binocular goggles, microphone (NordicNeuroLab, Norway). Spectral acoustic features (processed in Wavepad, praat and wavesurfer) of recorded verbal output (during MRI & outside) were fed in SVM for computing
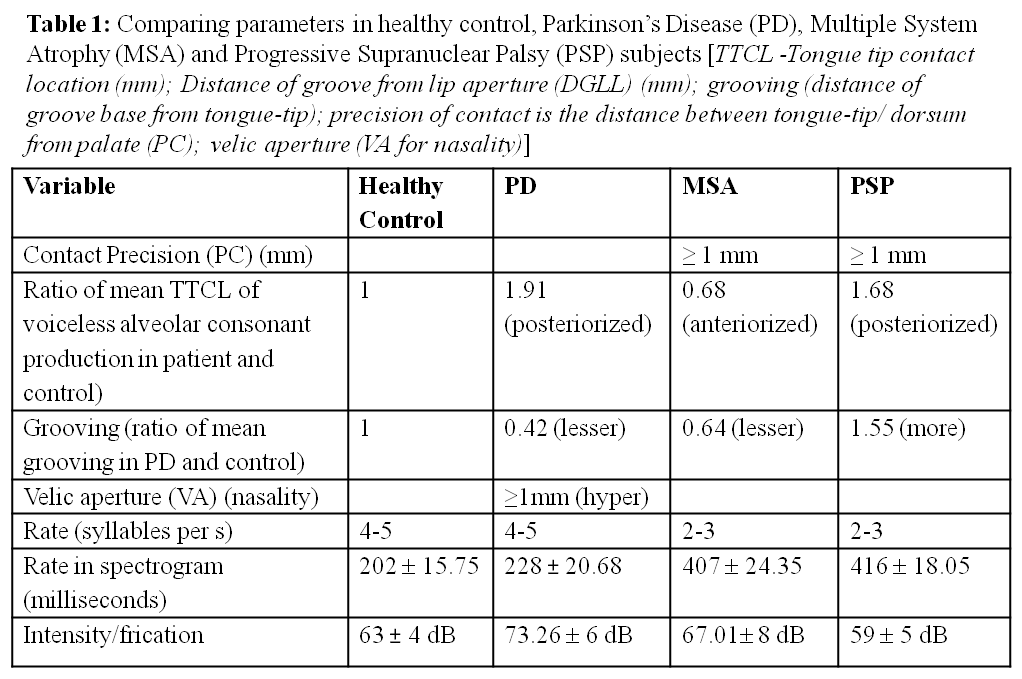
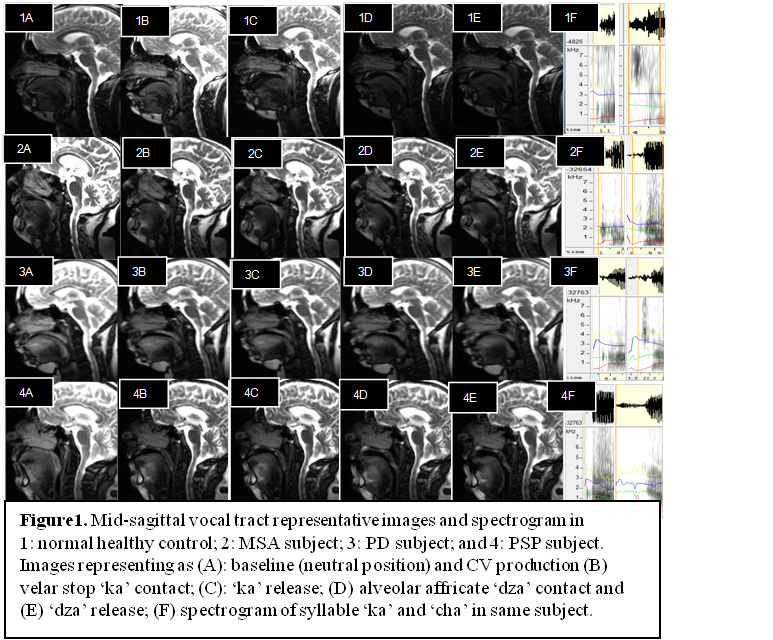
Results: MR images show imprecise velar constriction (PC>1mm), incomplete release and slow rate in MSA and PSP whereas imprecise and equal rate in PD. Contact/release calculated was 2-3sps (syllables per second) in MSA and PSP whereas in PD and control was 4-5sps similar to spectrogram analysis (Table1;Fig1). Affricate production in PD was posterorized, incomplete (PC>1mm) and lesser tongue body grooving. In MSA constriction was incomplete, anteriorized with less grooving and in PSP was posteriorized with more grooving. In PD observed hypernasality with VA>1mm. Pharyngeal, laryngeal shaping revealed vocal-cord vibration (Fig1D) but axial view would have been better. Compared to healthy control less grooving with more intensity/frication in PD and more grooving with less intensity/frication in PSP.[table1][figure1]
Conclusions: Dynamic MRI and automated acoustic features analysis increased efficacy and reduced time-cost of differential diagnosis
References: [1] Fu M, Zhao B, Carignan C, Shosted RK, et al, 2015. High-Resolution Dynamic Speech Imaging with Joint Low-Rank and Sparsity Constraints. Magn Reson Med. 2015 May; 73(5): 1820–1832.
[2] Benba A, Abdelilah Jilbab A, Hammouch A, 2016. Voice analysis for detecting patients with Parkinson’s disease using the hybridization of the best acoustic features. Int J Electrical Engineering and Informatics, 8(1). DOI: 10.15676/ijeei.2016.8.1.8
To cite this abstract in AMA style:
S. GUDWANI, S.S. Kumaran, M. Behari. Differentiating Parkinsonism with Spatio-temporal dynamics (real-time MRI) and Acoustics of Speech (spectrogram) [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/differentiating-parkinsonism-with-spatio-temporal-dynamics-real-time-mri-and-acoustics-of-speech-spectrogram/. Accessed December 30, 2025.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/differentiating-parkinsonism-with-spatio-temporal-dynamics-real-time-mri-and-acoustics-of-speech-spectrogram/