Session Information
Date: Monday, June 5, 2017
Session Title: Parkinsonism, MSA, PSP (Secondary and Parkinsonism-Plus)
Session Time: 1:45pm-3:15pm
Location: Exhibit Hall C
Objective: The description of differential diagnostic features of PSP and PD in order to improve the diagnosis and the differential diagnosis of these diseases.
Background: PSP is a disease of later life that is currently regarded as a form of neurodegenerative tauopathy (1). The clinical diagnosis of PSP relies on the identification of characteristic signs and symptoms (2).
Methods: 108 patients with idiopathic PD and 9 PSP patients were questioned. Average duration of PD was 4.0±1.68 years, and PSP was 4.0±1.94 years.
Results: –
Conclusions: PSP was characterized by later age of onset as compared with PD (p<0.04). The vast majority of PSP cases were characterized by bilateral onset (88.89%). Motor asymmetry was significantly more pronounced in PD, compared with PSP (p<0.001).
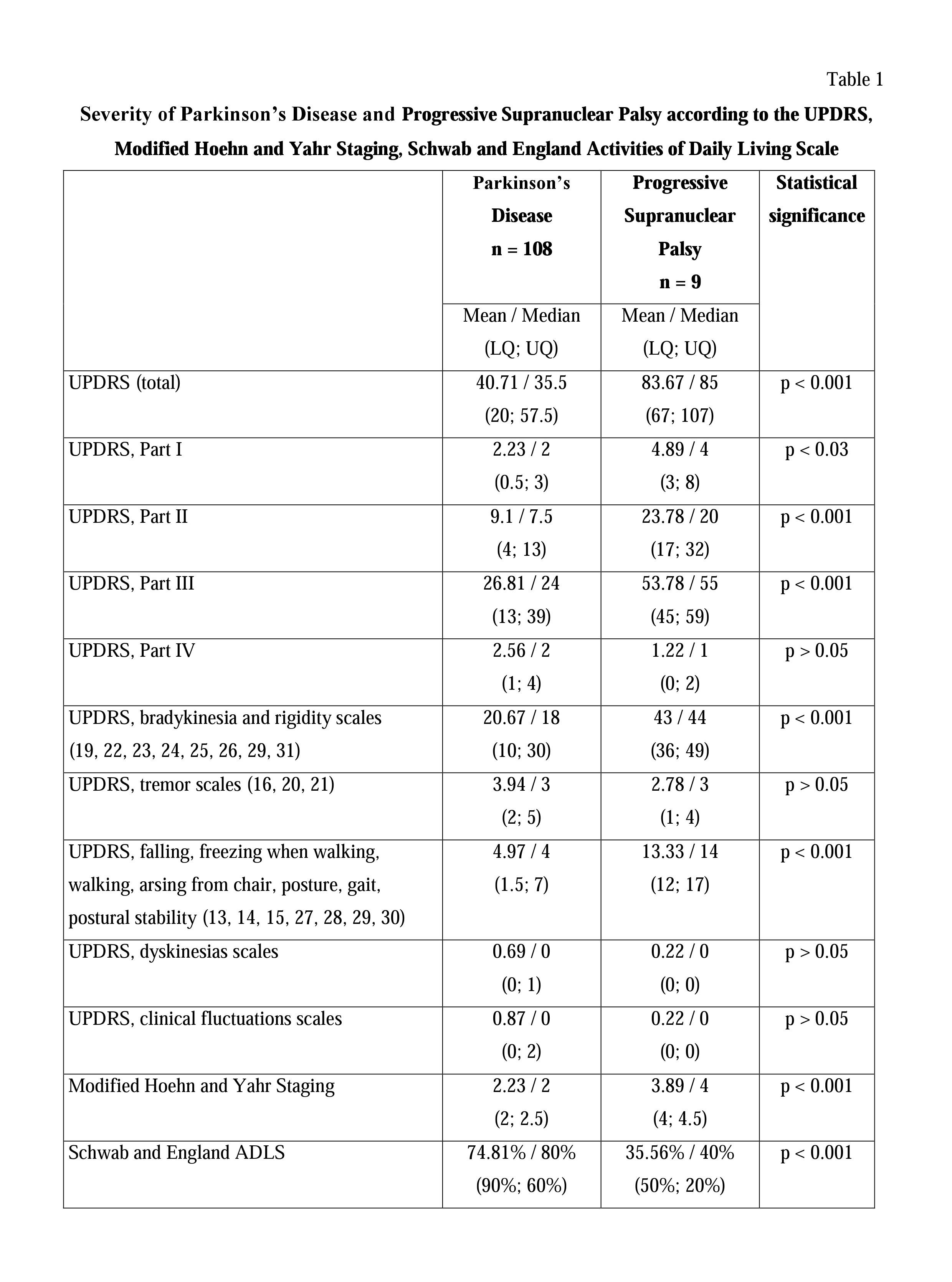
Average UPDRS scores, the Modified Hoehn and Yahr Staging and the Schwab and England ADL Scale in PSP patients significantly exceeded than in PD patients. A similar picture was observed with calculating I, II and III parts of UPDRS scores, bradykinesia and rigidity scales of UPDRS, and falling, freezing when walking, walking, arsing from chair, posture, gait, postural stability scales of UPDRS. [table1]
There was vertical gaze palsy in all PSP patients.
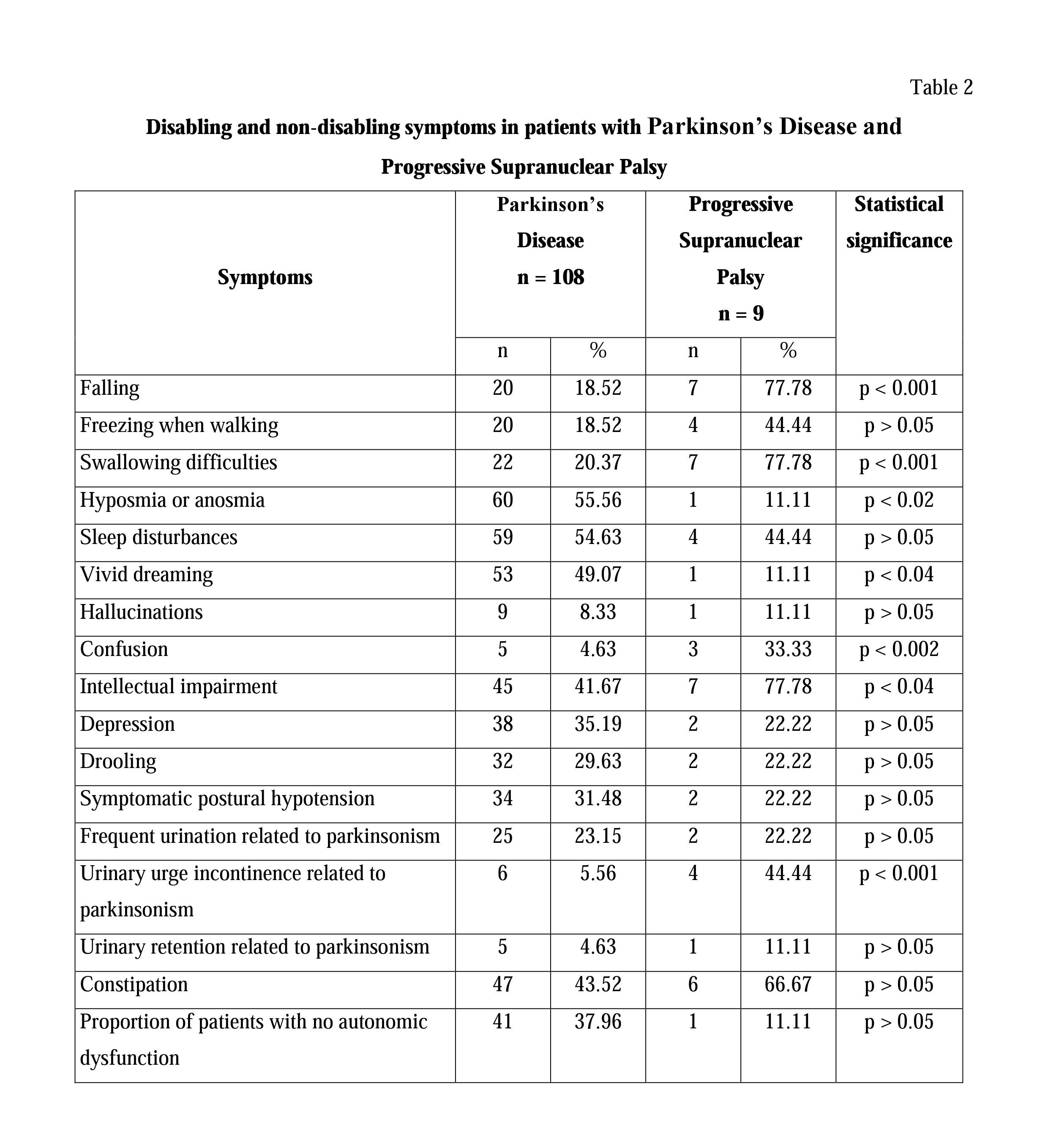
Falling within one year of parkinsonism was not characteristic of PD, but was found in 66.67% of PSP patients. Falling, intellectual impairment, confusion and urinary urge incontinence were statistically more common in PSP patients, compared with PD patients. Vivid dreaming and hyposmia were significantly more common in PD patients. [table2]
Severe swallowing difficulties were not characteristic of PD, but were a common signs of PSP (0.43% vs 44.44%; p<0.001). The presence and severity of swallowing difficulties can be considered as a differential diagnostic factor between PD and PSP, in early stages of the disease. The results of the videofluoroscopic swallowing study (VFSS) in patients with PSP mainly identified impairments of the pharyngeal phase of swallowing, leading to aspiration of food. The results obtained by using the VFSS, do not always correlate with clinical data and more severe disturbances were often found by using the VFSS.
The vast majority of PD patients (97.84%) experienced excellent, good, or moderate effect of levodopa. Unlike PD, we observed mild therapeutic effect of levodopa in 33.33% cases of PSP. Levodopa (800-1200 mg daily) was ineffective in 66.67% of PSP patients.
References:
- Chen AL, Riley DE, King SA, Joshi AC, Serra A, Liao K, … & Leigh RJ. The disturbance of gaze in progressive supranuclear palsy: implications for pathogenesis. Frontiers in neurology. 2010;1:147.
- Williams DR, de Silva R, Paviour DC, Pittman A, Watt HC, Kilford L, … & Lees AJ. Characteristics of two distinct clinical phenotypes in pathologically proven progressive supranuclear palsy: Richardson’s syndrome and PSP-parkinsonism. Brain. 2005;128(6):1247-1258.
To cite this abstract in AMA style:
Y. Trufanov. Differential diagnosis of Parkinson’s Disease and Progressive Supranuclear Palsy [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/differential-diagnosis-of-parkinsons-disease-and-progressive-supranuclear-palsy/. Accessed December 28, 2025.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/differential-diagnosis-of-parkinsons-disease-and-progressive-supranuclear-palsy/