Session Information
Date: Monday, June 5, 2017
Session Title: Parkinsonism, MSA, PSP (Secondary and Parkinsonism-Plus)
Session Time: 1:45pm-3:15pm
Location: Exhibit Hall C
Objective:
To report a case series of 4 patients with the PSP-C phenotype.
Background:
Ataxia is an exclusion criteria for the diagnosis of PSP. PSP-C, which has prominent cerebellar signs at presentation, is a rare phenotype that has been identified from autopsy series1. The clinical phenotype has not been well characterized at the early stage.
Methods:
Observational case series of patients with the clinical phenotype of PSP-C.
Results:
Demographics:
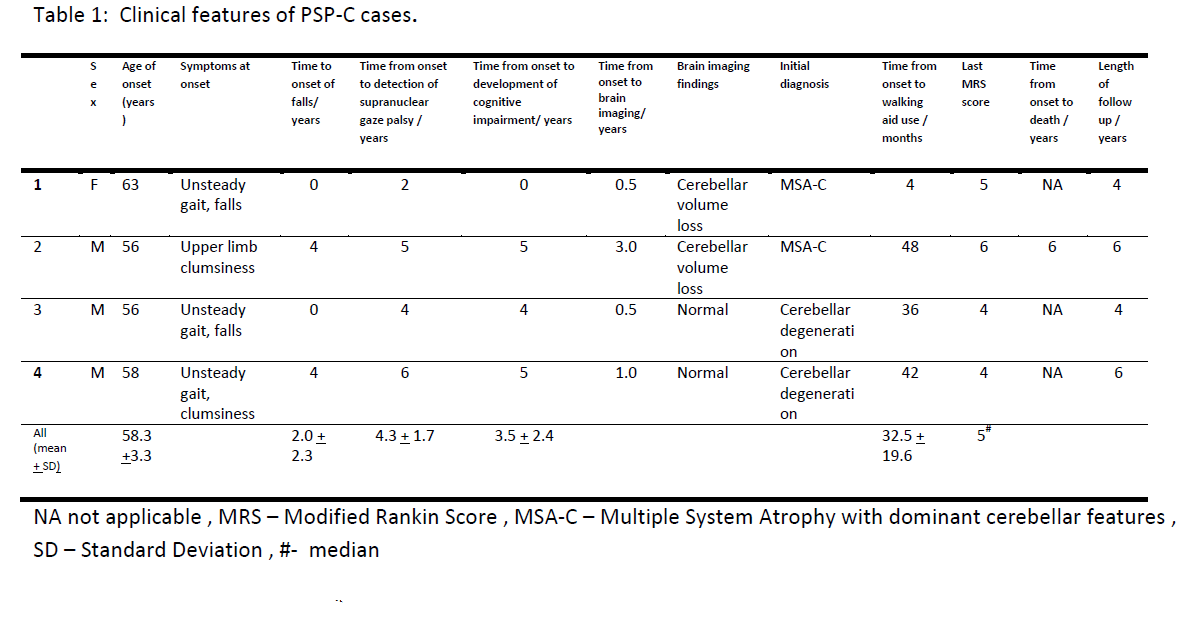
4 patients (3 males and 1 female) with PSP-C were identified and summarized in table 1. The average age of onset was 58.3 + 3.3 years. All tested negative for the Spinocerebellar Ataxia (SCA) types 1,2,3,6 and Dentatorubral-pallidoluysian atrophy (DRPLA). The average time from onset to falls, supranuclear gaze palsy and cognitive impairment was 2.0 + 2.3 years, 4.3 + 1.7 years and 3.5 + 2.4 years respectively. None developed dysautonomia. Radiological features suggestive of MSA-C were not detected.
Conclusions:
We present a case series of 4 patients with PSP-C. Our patients presented with gait disturbance and truncal ataxia followed by supranuclear gaze palsy in the absence of dysautonomia and absence of the hot cross bun sign on imaging which is similar to the Japanese series identified at postmortem. With disease progression, limb ataxia was masked by the marked rigidity.
It has been suggested that PSP-C is slowly progressive. However, the time from onset to the occurrence of falls, cognitive impairment and supranuclear gaze palsy was rapid and follows most closely the trajectory of the Richardson-Steele phenotype of PSP which has the worst prognosis.
The average onset of supranuclear palsy from initial symptoms was 4.3 + 1.7 years, with one patient developing supranuclear gaze palsy 6 years after the onset. In contrast, supranuclear gaze palsy was detected in only 1 of the 5 Western cases at ante mortem despite a long disease duration2. These patients had a benign clinical course with ataxia as the only finding. An unknown proportion of adult onset cerebellar ataxia could thus be cases of PSP-C that do not develop supranuclear palsy ante mortem. Proposed diagnostic criteria should reflect the wide variability in the onset of supranuclear gaze palsy.
We were able to characterize the PSP-C phenotype and the cases described are clinically similar to the autopsy proven Japanese cases. Other differentials to consider include Parkinsonism associated with POLG1 mitochondrial mutations, spinocerebellar ataxias with ophthalmoparesis and Niemann-Pick disease type C but these have a different clinical presentation.
In conclusion, clinicians should be vigilant to this diagnostic possibility as supranuclear gaze palsy may manifest many years after the initial onset of cerebellar ataxia.
References: 1. Kanazawa M, Shimohata T, Toyoshima Y, Tada M, Kakita A, Morita T, et al. Cerebellar involvement in progressive supranuclear palsy: A clinicopathological study. Mov Disord 2009;24(9):1312-1318. 2. Koga S, Josephs KA, Ogaki K, Labbe C, Uitti RJ, Graff-Radford N, et al. Cerebellar ataxia in progressive supranuclear palsy: An autopsy study of PSP-C. Mov Disord;31(5):653-662
To cite this abstract in AMA style:
Z. Xu, T. Lim, W.L. Au, L. Tan. The clinical phenotype of progressive supranuclear gaze palsy with predominant cerebellar ataxia (PSP-C): a case series [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/the-clinical-phenotype-of-progressive-supranuclear-gaze-palsy-with-predominant-cerebellar-ataxia-psp-c-a-case-series/. Accessed April 1, 2025.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/the-clinical-phenotype-of-progressive-supranuclear-gaze-palsy-with-predominant-cerebellar-ataxia-psp-c-a-case-series/